Overview
The Patient Protection and Affordable Care Act (ACA) included a critical provision to increase Medicaid payment for primary care services to Medicare levels in calendar years 2013-2014. This provision, championed by the AAP, raised Medicaid payment for evaluation and management (E/M) and immunization administration services provided by primary care physicians with specialty designations of pediatric medicine, family medicine, and/or general internal medicine during those 2 years. Subspecialists boarded under 1 of the aforementioned specialty member boards–as well as other subspecialists practicing primary care who could support this with a claims history–were also eligible for the Medicaid payment increase.
The increase applied to fee-for-service care as well as care provided in Medicaid managed care organization (MCO) structures. Physicians were required to self-attest eligibility for the payment increase to their state Medicaid programs in order to receive it, and while retroactive payment at increased levels was available to January 1, 2013, some states implemented self-attestation deadlines to receive these payments.
While the ACA Medicaid payment increase ended December 31, 2014 without a renewal from Congress, a number of states have acted to extend the increase with state funds.
AAP Position
- Medicaid payment is set by each state and has historically been low. The AAP supports efforts at the state and federal levels to raise Medicaid payment rates for all physician services to those that are at least equivalent with Medicare rates.
- Low Medicaid payment negatively impacts the ability of pediatricians to participate in the program and impedes access to care for enrollees.
- In November 2015, CMS issued a long-awaited “equal access” rule, requiring states to document access to care in the Medicaid program through an access monitoring review plan. A separate analysis is required when a state proposes a rate decrease.
- In March 2018, CMS released a proposed change that would exempt states from the equal access rule if they had a managed care penetration over 85% or if reductions to payments were of a certain size. In July 2019, CMS proposed eliminating the access monitoring review plan requirement altogether.
Facts
- The ACA Medicaid payment increase applied to E/M codes 99201 through 99499 as well as vaccine administration codes 90460, 90461, 90472, 90473, and 90474, or their successor codes. These include codes not recognized for payment by Medicare but assigned Relative Value Units (RVUs).
- States using state dollars to fund Medicaid payment rate increases are not required to follow the rules that were originally outlined in the ACA. States are free to implement this policy however they deem appropriate.
- New literature demonstrates that the ACA Medicaid payment increase had a positive impact on access to care, with office based primary care pediatricians increasing their participation in the Medicaid program during these years (Pediatrics, January 2018).
Progress
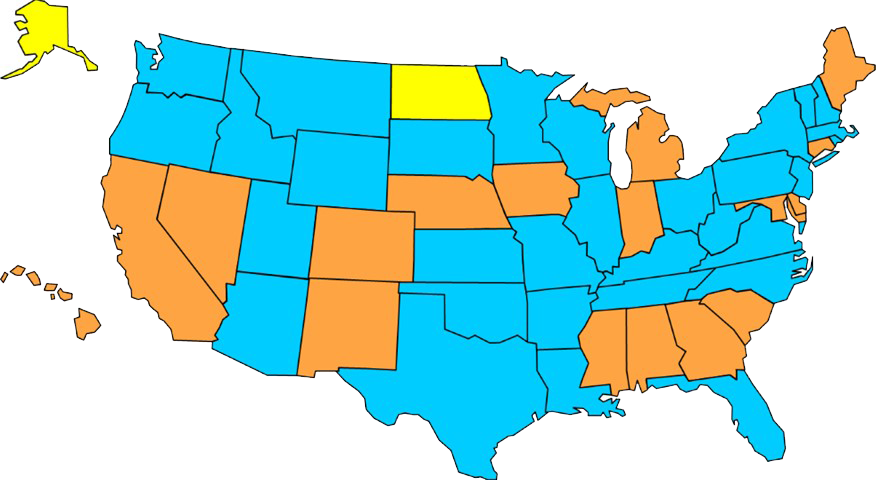
- 17 states using state dollars to extend the increase in State Fiscal Year (SFY) 2019*
- 31 states not using state dollars to extend the increase in SFY 2019
- 2 states Medicaid rates at or higher than Medicare rates
*Implementation varies by state. For example Michigan Medicaid rates have been increased to 78% of Medicare rates.