Last Updated
09/09/2022
The coronavirus 2019 (COVID-19) pandemic has created profound challenges for communities, families, and individuals. While some of the challenges that characterized the initial phase of the pandemic have eased in their intensity, such as the need for quarantine and physical isolation, continued guidance on the effects of and response to the virus and the pandemic is needed.
This guidance applies to children and adolescents who are participating in and/or returning to physical activity, inclusive of but not limited to, organized sports and physical education class within school. Pediatricians should consider any children or adolescents who participate in any physical activity, organized or not, to fall within the context of this guidance.
This update clarifies CDC guidance for quarantine. isolation, and community levels as it relates to sports and provides guidelines for return to physical activity after a COVID-19 diagnosis.
Approximately 35 to 45 million youth 6 to 18 years of age participate in some form of athletics. The COVID-19 pandemic has affected many aspects of the lives of children and families, including youth sport activity. As children present for health supervision visits and preparticipation physical evaluations, parents and athletes likely will ask questions about how best to ensure safety when considering a return to sports participation and physical activity. This guidance is intended for pediatricians to inform families on how to mitigate risk and prevent the spread of SARS-CoV-2, the virus that causes COVID-19, to others within sports and other physical activities. Pediatricians should also refer to their state regulations and guidance associated with return to sports as states are allowing practice and competition to resume at different stages.
Sports preparticipation examination and preparing for the season
All children should have an annual health supervision visit, which ideally incorporates the preparticipation physical evaluation (PPE; also known as the sports physical). Pediatricians should inquire about any known SARS-CoV-2 infections and vaccination/booster status since the last evaluation and should document it within the patient’s medical record. The AAP strongly recommends that all people who are eligible should receive the primary series of the COVID-19 vaccine, receive booster doses when recommended, and continue to follow transmission mitigation recommendations as described by the CDC.
The PPE History form and Physical Examination form have been revised to incorporate questions regarding COVID-19 history and COVID-19 vaccination status. As part of the PPE, appropriate screening and guidance back to physical activity should be provided as outlined in this document. Please note: Athletes who have a current PPE (per state and local guidance) on file should not need to complete another examination or history form.
Transmission Mitigation
SARS-CoV-2 transmission among athletes has been documented in the sports setting, with indoor sports likely bearing the greatest risk, especially wrestling, ice hockey, and basketball. Consideration should be made for increased ventilation in indoor settings via opening doors or windows when safe.
Most transmission associated with outdoor sports has been related to off-field activities, such as sharing meals and during transportation in private vehicles where people were unmasked or partially masked. SARS-CoV-2 infection rates for outdoor sports are likely to reflect local community infection rates. However, with the emergence of new SARS-CoV-2 variants with higher infectivity rates, transmission during outdoor on-field activities is of greater concern.
Children and adolescents with any signs or symptoms of SARS-CoV-2 infection should not attend practices or competition. They should consult their pediatrician for testing guidance and notify their coach, athletic trainer, and/or school administrator of their signs/symptoms.
All individuals who are exposed to someone with SARS-CoV-2 should follow the current CDC recommendations for a known exposure.
Use of face masks
The use of a well-fitting face mask consistently reduces the spread of SARS-CoV-2 virus.
At a “high” level of community COVID-19 transmission, it is strongly recommended that athletes, coaches, officials, and spectators wear a face mask indoors, even if they are vaccinated and boosted.
When a county is in the “medium” level, a face mask would be recommended for indoors if an athlete or someone on the team or within their home is immunocompromised or considered high risk.
Coaches and other club/school officials should monitor proper use and encourage all athletes to have a well-fitting face mask in place in accordance with the above guidance and local recommendations. CDC guidance on selecting a proper face mask can be found here.
Special considerations may be appropriate when there is an increased risk of heat-related illness. Children younger than 2 years old should not wear a face mask. Younger athletes may find wearing a face mask challenging and may need to be reminded and/or assisted by parents/coaches. People should be reminded not to touch the front of the face mask and remove it from the face touching only the straps whenever possible. It is important to recognize that face masks have been shown to be well tolerated by most people who wear them for exercise.
Proper face mask use during indoor sports decreases risk of SARS-CoV-2 transmission, and individuals may choose to wear a face mask at any time to help mitigate risk of infection. If a face mask is indicated for indoor sports activity, the mask should be worn consistently and correctly, including during play. If the face mask is removed for a break, the athlete should remain at least 3 feet away from all other people. The mask may need to be removed under certain circumstances.
Face masks should not be worn during certain situations in competitive cheerleading and gymnastics because of the risk that the mask may get caught on objects and become a choking hazard or accidentally impair vision. For competitive cheer, face mask use should be emphasized when individuals are within 3 feet of each other and risk for mask displacement is low. For gymnastics, the face mask should be removed when athletes are on the apparatus. It should be replaced as soon as the exercise is completed.
During wrestling contact, a face mask could become a choking hazard and is discouraged unless an adult coach or official is closely monitoring for safety purposes. People who swim/dive/participate in water sports should not wear a face mask while they are in the water, because a wet face mask may be more difficult to breathe through. Any face mask that becomes saturated with sweat should be changed immediately. If other sport-specific scenarios arise in which a face mask may obstruct a person’s view or become a choking hazard, league officials should use their discretion to determine whether risk of mask use outweighs risk of SARS-CoV-2 transmission.
Child/adolescent with positive COVID-19 test
If a child/adolescent tests positive for COVID-19, team officials should be notified so appropriate notification can be performed according to local policy and protocols. All individuals who test positive should follow CDC guidance for isolation. This guidance includes the following:
- Regardless of vaccination status, the COVID-19-positive individual should isolate at home for a minimum of 5 days.
- After a full 5 days have passed from symptom onset or positive test result, the individual may end isolation if asymptomatic or symptoms are improving. Individuals with fever must remain in isolation until a minimum of 24 hours have passed while off fever-reducing medication.
- All individuals who test positive for COVID-19 must mask when around others for a full 10-day period. This includes with all physical activity.
Evaluation for Resumption of Physical Activity/sports Activity for a Child/Adolescent With COVID-19
Do all children who have experienced a SARS-CoV-2 infection, whether symptomatic or not, require a follow-up visit?
All patients who test positive for a SARS-CoV-2 infection should have at least one follow-up conversation or visit with their primary care medical home. We recommend that this encounter occur either prior to resuming sports/physical activity or within 2 to 4 weeks of a positive SARS-CoV-2 test, whichever is sooner. The medical home is a trusted source of information for patients and families, including information about asymptomatic infection or COVID-19 disease and its sequelae.
Acute COVID-19 severity does not necessarily predict subsequent or ongoing signs or symptoms. Recent literature has reported a much lower incidence of myocarditis, 0.5% to 3%, than earlier in the pandemic. However, myocarditis has been documented even in people with COVID-19 who were asymptomatic or had mild infections.
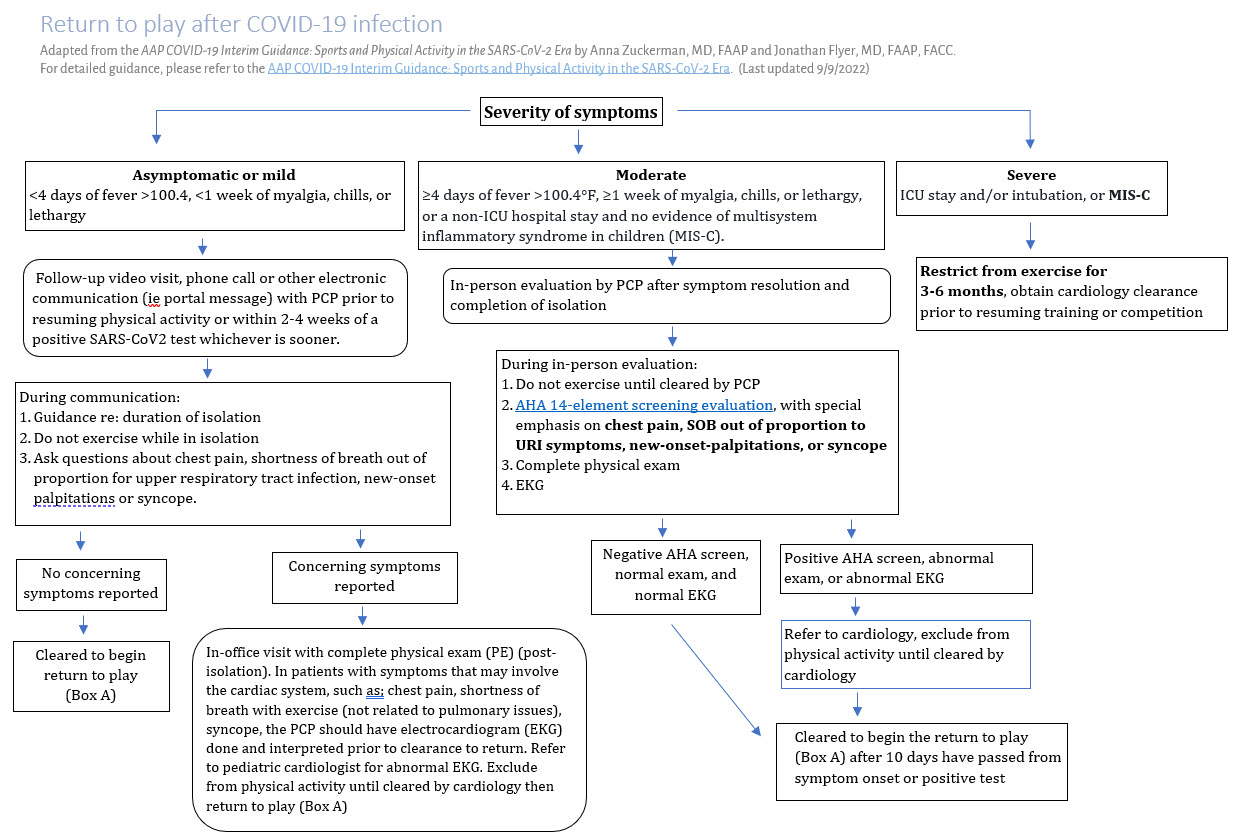
For asymptomatic infection or mild disease severity (<4 days of fever >100.4°F; <1 week of myalgia, chills, and lethargy), a follow-up video visit, phone call, or other electronic communication (eg. portal message) is recommended. Individuals who are asymptomatic or have mild symptoms who complete their 5-day isolation should be fever free off all fever-reducing medication and have improving symptoms for a minimum of 1 day prior to beginning a return to physical activity progression. All athletes and their parents should be provided with guidance to monitor for signs/symptoms concerning for myocarditis as they return to physical activity. This includes monitoring for any onset of chest pain, shortness of breath out of proportion for upper respiratory tract infection, new-onset palpitations, or syncope. These are indications for stopping physical activity and seeking immediate medical care; consultation with a pediatric cardiologist should be encouraged.
For those with moderate symptoms of COVID-19 (≥4 days of fever >100.4°F, ≥1 week of myalgia, chills, or lethargy, or a non-ICU hospital stay and no evidence of multisystem inflammatory syndrome in children [MIS-C]), an evaluation by their primary care physician (PCP) is recommended, as these patients may be at greater risk for subsequent cardiovascular disease. People who test positive for SARS-CoV-2 should not exercise until they are cleared by a physician. PCP evaluation is currently recommended after symptom resolution and completion of isolation. The PCP will review the American Heart Association 14-element screening evaluation with special emphasis on cardiac symptoms including chest pain, shortness of breath out of proportion for upper respiratory tract infection, new-onset palpitations, or syncope and perform a complete physical examination and an EKG. If cardiac workup is negative, gradual return to physical activity may be initiated after 10 days have passed from the date of the positive test result, and a minimum of 1 day of symptom resolution (excluding loss of taste/smell) has occurred off fever-reducing medicine. If cardiac sign/symptom screening is positive or EKG is abnormal, referral to a cardiologist is recommended. The cardiologist may consider ordering a troponin test and an echocardiogram at the time of acute infection. Depending on the patient’s symptoms and their duration, additional testing including a Holter monitor, exercise stress testing, or cardiac magnetic resonance imaging (MRI) may be considered
Individuals who have moderate symptoms may not exit their isolation until a minimum of 5 days have passed, symptoms are improving, and they are fever free off all fever-reducing medication for a minimum of 1 day. Physician clearance is required prior to beginning a return to physical activity progression, and a minimum of 1 day of being fever free off fever-reducing medication and improving symptoms is recommended prior to starting a return to physical activity progression. All athletes and their parents should be provided with guidance to monitor for signs/symptoms concerning for myocarditis as they return to physical activity. This includes monitoring for any onset of chest pain, shortness of breath out of proportion for upper respiratory tract infection, new-onset palpitations, or syncope. These are indications for stopping physical activity and seeking immediate medical care; consultation with a pediatric cardiologist should be encouraged.
For children and adolescents with severe COVID-19 symptoms (ICU stay and/or intubation) or MIS-C, it is recommended they be restricted from exercise for a minimum of 3 to 6 months and obtain cardiology clearance prior to resuming training or competition. Coordination of follow-up cardiology care should be arranged prior to hospital discharge. Other testing may be ordered based on the child or adolescent’s signs and symptoms.
For children and adolescents with a history of SARS-CoV-2 infection who have already advanced back to physical activity/sports on their own and do not have any abnormal signs/symptoms, no further workup is necessary. It is recommended that these children and adolescents update their pediatrician’s office via a phone call to ensure the history of SARS-CoV-2 infection is added to their medical record.
After testing positive for SARS-CoV-2, how should children and adolescents return to physical activity and/or sports?
The AAP recommends not returning to sports until children or adolescents have completed isolation, the minimum amount of symptom-free time (as outlined above) has passed, they can perform normal activities of daily living (ADLs), they display no concerning signs/symptoms, and a physician evaluation has been completed if indicated.
Individuals who exit isolation after 5 days post-symptom onset or positive test should wear a face mask for all activity around other individuals for a total of 10 days from onset of symptoms or positive COVID-19 test, including for all physical activity. If a face mask cannot be worn during their sport (ie, swimming/diving), these individuals may participate in other physical activity as part of their progression until their 10 days has been completed and then can return to their sport without a mask.
All children younger than 12 years with COVID-19 may progress back to sports/physical education classes according to their own tolerance once above steps for isolation and clearance have been completed.
Individuals who are 12 years and older should perform the following progression once isolation is completed and physician clearance has been obtained if indicated:
- Asymptomatic/mild symptoms: Minimum 1 day symptom free (excluding loss of taste/smell), tolerating ADLs, 1 day of practice prior to return to games is recommended . A face mask should be worn for ALL physical activity, including games or scrimmages, until 10 full days from positive test or symptom onset have passed.
- Moderate symptoms: Minimum 1 day symptom free (excluding loss of taste/smell), tolerating ADLs, one light practice or 30 minutes minimum of cardiovascular exercise on own, and 1 full practice prior to games is recommended. A face mask should be worn for ALL physical activity, including games or scrimmages, until 10 full days from positive test or symptom onset have passed.
All children and adolescents and their parents/caregivers should be educated to monitor for chest pain, shortness of breath out of proportion for upper respiratory tract infection, new-onset palpitations, or syncope when returning to exercise. If any of these signs and/or symptoms occur, the AAP recommends immediately stopping exercise and seeing a pediatrician for an in-person assessment, and consideration should be given for pediatric cardiology consultation.
AAP Resources
- Preparticipation Physical Evaluation, 5th Edition Monograph
- Organized Sports for Children, Preadolescents, and Adolescents
- Overuse Injuries, Overtraining, and Burnout in Child and Adolescent Athletes
- Physical Activity Assessment and Counseling in Pediatric Clinical Settings
- COVID-19 Planning Considerations: Guidance for School Re-entry
- COVID-19 and Safe Transportation in Motor Vehicles
- COVID-19 Testing Guidance
- Cloth Face Coverings
- Supporting Healthy Nutrition and Physical Activity During the COVID-19 Pandemic
- Coding During the COVID-19 Public Health Emergency (PHE)
- COVID-19 Vaccine for Children
- PPE History Form
- PPE Physical Examination Form
Information for Families from HealthyChildren.org
- Cloth Face Coverings During Sports
- Mask Mythbusters: 5 Common Misconceptions about Kids & Cloth Face Coverings
- Youth Sports & COVID-19: Understanding the Risks
- Youth Sports Participation During COVID-19: A Safety Checklist
Additional Information
- American Medical Society for Sports Medicine: Interim Guidance on the Pre-participation Physical Exam for Athletes during the SARS-CoV-2 Pandemic
- Centers for Disease Control and Prevention: Consideration for Youth Sports
- World Health Organization: COVID-19 and Staying Active
- American College of Cardiology: Returning To Play After Coronavirus Infection: Pediatric Cardiologists' Perspective
- Centers for Disease Control and Prevention: When You’ve Been Fully Vaccinated
Interim Guidance Disclaimer: The COVID-19 clinical interim guidance provided here has been updated based on current evidence and information available at the time of publishing. Additional evidence may be available beyond the date of publishing.
Last Updated
09/09/2022
Source
American Academy of Pediatrics