Overview
The Affordable Care Act (ACA) requires the establishment of an “essential health benefits (EHB) package” for certain health insurance plans including qualified health plans (QHPs) and the Medicaid expansion population. Under federal guidance, states were allowed to define and update the EHB package by choosing among 4 benchmarks and supplementing those benchmarks to ensure all 10 categories of EHB are met. In 2018, a new federal rule gave states new authority to change EHB benchmarks by choosing from new benchmark options and substituting benefits between categories. These changes allow states to provide fewer benefits in EHB packages starting in 2020. The new rule also makes EHB benchmark selection an annual activity.
If states choose a less robust benchmark, children and families in individual and small group coverage will have fewer needed benefits covered and may be subject to higher out-of-pocket costs. Large group and self-insured plans could also be impacted by these changes, as ACA annual and lifetime dollar limits and out-of-pocket spending protections are connected to EHB benefits. If a service is removed from EHB, these protections would no longer apply to that service.
AAP Position
- EHB benefit packages should not be weakened by state selection of a less robust benchmark option or by allowing substitution between categories. If substitutions are made, they should be extremely limited and ensure that benefit packages meet the needs of children.
- Medicaid’s Early and Periodic Screening, Diagnosis and Treatment (EPSDT) guarantee or the Children’s Health Insurance Program’s (CHIP) benefit package should be the benchmark plan for children, to ensure all children receive the care they need.
- Habilitation services should be offered at parity with rehabilitation services.
- In instances where states need to supplement pediatric oral or vision services in the EHB benchmark plan, states should use the most robust option available for these services.
Facts
- The 10 categories of benefits in an EHB package are: 1) ambulatory patient services, 2) emergency services, 3) hospitalization, 4) maternity and newborn care, 5) mental health and substance use disorder services, 6) prescription drugs, 7) rehabilitative and habilitative services and devices, 8) lab services, 9) preventive and wellness services and chronic disease management, and 10) pediatric services, including oral and vision care.
- States that do not change their benchmark plans will continue to use their benchmark selection from the previous year. Under the 2018 rule, states can now select EHB benchmark plans by:
- Selecting an EHB benchmark plan from another state
- Replacing one or more existing EHB benefit categories with the same categories of benefits
used in another state’s EHB benchmark plan; - Selecting a new set of benefits that would provide the state’s EHB benchmark.
- The new federal rule creates a “generosity standard” that imposes a maximum set of benefits for all state EHB plans starting in 2020; it requires that no EHB package include more generous benefits by actuarial value than the most generous of the 10 benchmark plan option available to the state.
Progress
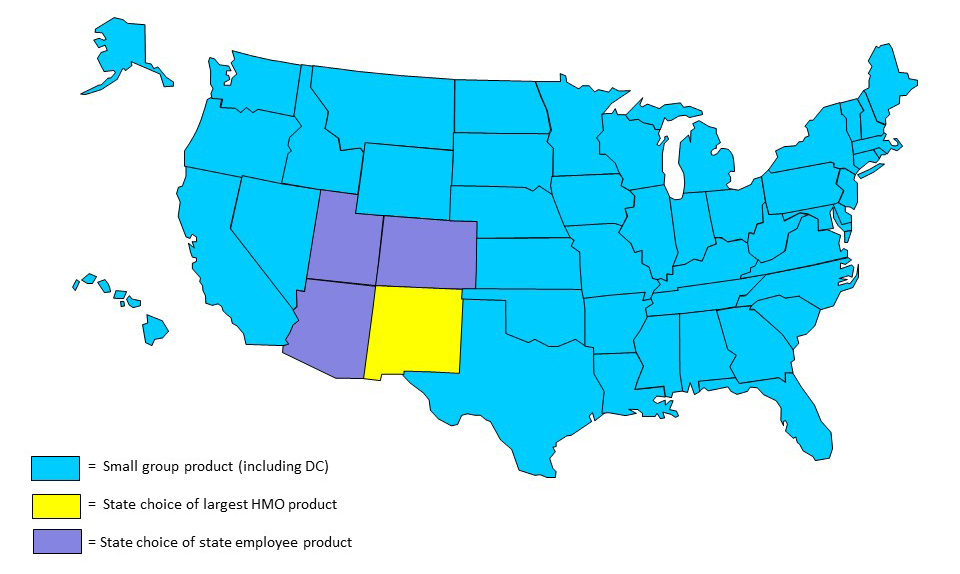
[State choices for 2020 plan year]
- 46 states and DC – largest small group product
- 1 state – largest HMO product
- 3 states – state employee product
For information on current law or pending legislation in your state, please contact AAP State Advocacy at [email protected].
More
- Essential Health Benefits and Other ACA Protections | New Rule Poses Threat to Benefits for Children and Families
- State Roles in Defining Essential Health Benefits
- A Comparative Review of Essential Health Benefits Pertinent to Children in Large Federal, State, and Small Group Health Insurance Plans: Implications for Selecting Benchmark Plans