As suicide research has advanced, it has become clear that suicide risk includes a complex set of factors at the individual, relationship, community, and societal level, contributing to a life-threating health crisis. As is the case with many health-related causes of death, a robust public health strategy can be effective in reducing morbidity and mortality.
Suicide among youth and young adults is a critical public health concern. Pediatric health clinicians have an important role to play in reducing the risk of suicide in this age group.
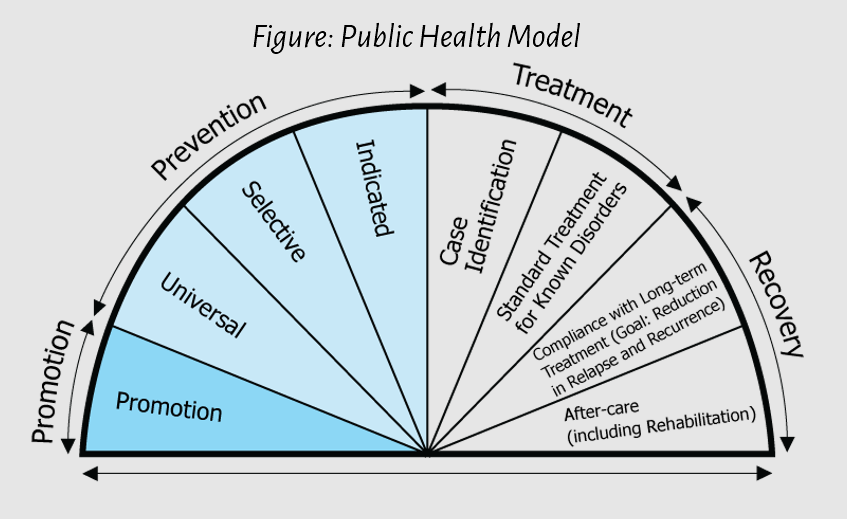
Optimal results can be achieved with a multi-layered approach to health outcome goals, including suicide prevention. When Promotion and Prevention efforts at all levels are strategic and sustained, and when Treatment and Recovery resources are well developed and accessible to the population, we have the best chance of reducing suicide mortality.
Source: Substance Abuse and Mental Health Services Administration (SAMHSA), used with permission. Please note that inclusion of SAMHSA content does not constitute or imply endorsement or recommendation by SAMHSA, the US Department of Health and Human Services, or the US Government.
Following a public health model, suicide prevention strategies can be implemented at 3 levels:
- Universal Strategies (ie, Primary Prevention): Suicide prevention efforts directed at the full population. These universal efforts include activities such as resilience and mental health promotion, safe media messaging, lethal means access reduction, increased access to high quality supports and mental health services, suicide risk screening in all healthcare settings, and suicide prevention education for all adults who work with youth
- Selective Strategies: Suicide prevention efforts focused on populations at elevated risk. These include training and skill-building with professionals who work with specific populations (eg, health care professionals, school personnel, coaches, corrections officers, or child welfare system personnel)
- Indicated Strategies: Suicide prevention efforts directed at individuals with the highest risk for suicide and applied during known timeframes when suicide risk is elevated. These include direct intervention and supports for youth who are at acute or non-acute risk for suicide and their families. An example of indicated suicide prevention is identifying patients with suicidal thoughts and/or current or previous suicidal behavior who then receive care coordination, caring follow-up contacts, and safety planning.
This Blueprint outlines universal, selective, and indicated strategies that pediatric health clinicians can take to prevent youth suicide in clinical, community, and advocacy settings. Throughout the Blueprint, an equity lens provides considerations for youth from marginalized or high-risk populations.
Youth Suicide Prevention: A Call to Action
Suicide is complex and tragic. But it can be prevented.
Pediatric health clinicians have a role to play at all levels of suicide prevention and intervention. Some examples are listed below:
- Universal Strategies (ie, Primary Prevention): These strategies can be offered to all audiences across settings. Examples include speaking out against stigma, raising awareness, and educating patients and families about mental health and suicide prevention
- Selective Prevention: Examples include screening patients in all healthcare settings for mental health concerns and suicide risk, facilitating a support group for at-risk youth, and partnering with schools to increase screening and support groups
- Indicated Prevention: Examples include actively checking-in with patients about suicidal thoughts and behavior, offering care coordination, safety plans and follow up when treating patients for high-risk conditions (eg, depression, anxiety, trauma, post-traumatic stress disorder (PTSD), eating disorders, other chronic medical conditions, pain, substance use, or experiencing a loss to suicide)
- Treatment: This includes optimizing treatment for any mental health condition and focusing on suicide risk as a separate but related clinical target. Examples include engaging with patients about their suicidal thoughts and providing specific clinical care steps, providing lethal means safety counseling to patients and families when suicide risk is identified. (See “Preventing Youth Suicide: Strategies for Clinical Settings” section of this Blueprint)
- Recovery: Examples include following up with and supporting patients, ensuring they are continuing with mental health treatment or therapy, and fostering family or community-based support following a mental health or suicidal crisis
This Blueprint is designed to support pediatric health clinicians in identifying and supporting youth at risk for suicide in clinical and community settings.
With the right knowledge and partnerships, we can all play a role in addressing youth suicide.
Last Updated
02/04/2022
Source
American Academy of Pediatrics