Children with EoE can present with a wide range of symptoms. Sometimes contributing to diagnostic confusion, many other conditions can mimic the symptoms of EoE, such as:
- Gastroesophageal reflux
- Gastroenteritis
- Constipation
- Functional dyspepsia
- Reflux hypersensitivity
- Globus
- Functional dysphagia
Symptoms can vary in frequency and severity. Given the broad differential diagnosis associated with these common pediatric symptoms, suspicion for EoE should be raised for any child with abnormal presentation or associated comorbid allergic conditions. Broadly, symptoms of EoE and evidence of esophageal dysfunction include:
- Dysphagia
- Recurrent emesis
- Recurrent or chronic abdominal pain
- Reflux
Other signs and symptoms include:
- Food impaction (Figure 1)
- Failure to progress with food introduction (infants and toddlers)
- Feeding difficulty at any age
- Heartburn
- Regurgitation
- Chest pain
- Odynophagia
- Abdominal pain
- Malnutrition
 Figure 1. Food impaction in a patient with EoE.
Figure 1. Food impaction in a patient with EoE.
From Adamiak T, Plati KF. Pediatric esophageal disorders: diagnosis and treatment of reflux and eosinophilic esophagitis. Pediatr Rev. 2018;39(3):392-402.
Symptoms can vary according to the age of the child (see Table 1). This is likely a function of esophageal fibrosis and remodeling, stricture formation and stenosis that may occur over time, but may also be attributed to the fact that older children are generally better able to articulate specific symptoms.
- For instance, food impaction is much more common in older children and adolescents and the absence of this should not preclude consideration of EoE in younger children.
Table 1. Signs and Symptoms of EoE by Age Group
|
General Age Group |
Signs and Symptoms |
|
Infants |
GERD-like symptoms, including:
|
|
Young children |
|
|
Adolescents |
|
|
Young adults |
|
Endoscopic Findings
EoE cannot be established or excluded based upon the macroscopic appearance of the esophagus. Children with EoE may have a normal appearing esophagus or one or more of the following findings at endoscopy:
- Esophageal rings
- Longitudinal furrows
- Exudate
- Edema (Figure 2)
- Stricture (Figure 3)
- Narrow-caliber esophagus
- Crepe paper esophagus
- Feline esophagus
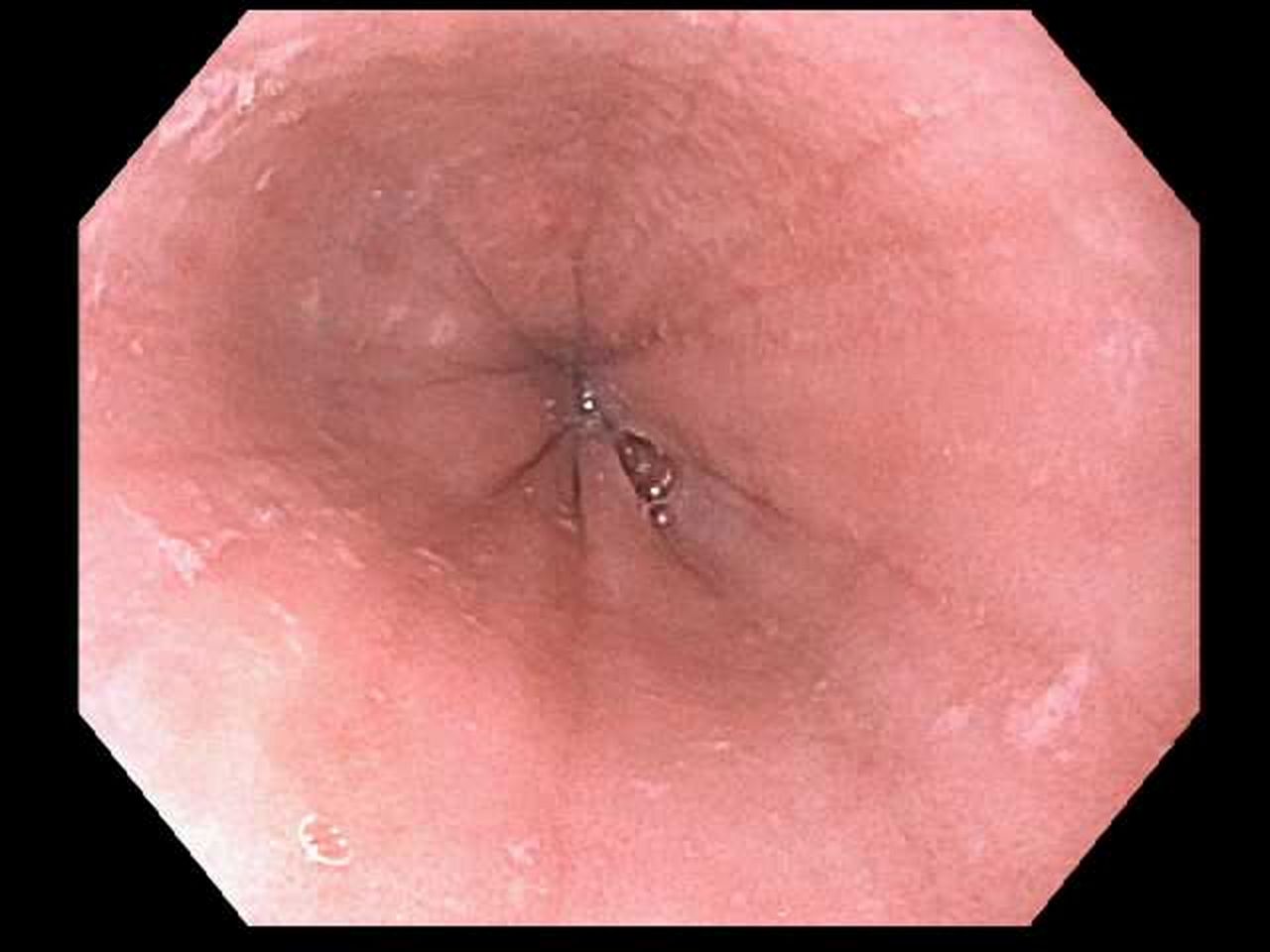 Figure 2. Mucosal edema, loss of vascular pattern, and linear furrows in a patient with eosinophilic esophagitis.
Figure 2. Mucosal edema, loss of vascular pattern, and linear furrows in a patient with eosinophilic esophagitis.
From Adamiak T, Plati KF. Pediatric esophageal disorders: diagnosis and treatment of reflux and eosinophilic esophagitis. Pediatr Rev. 2018;39(3):392-402.
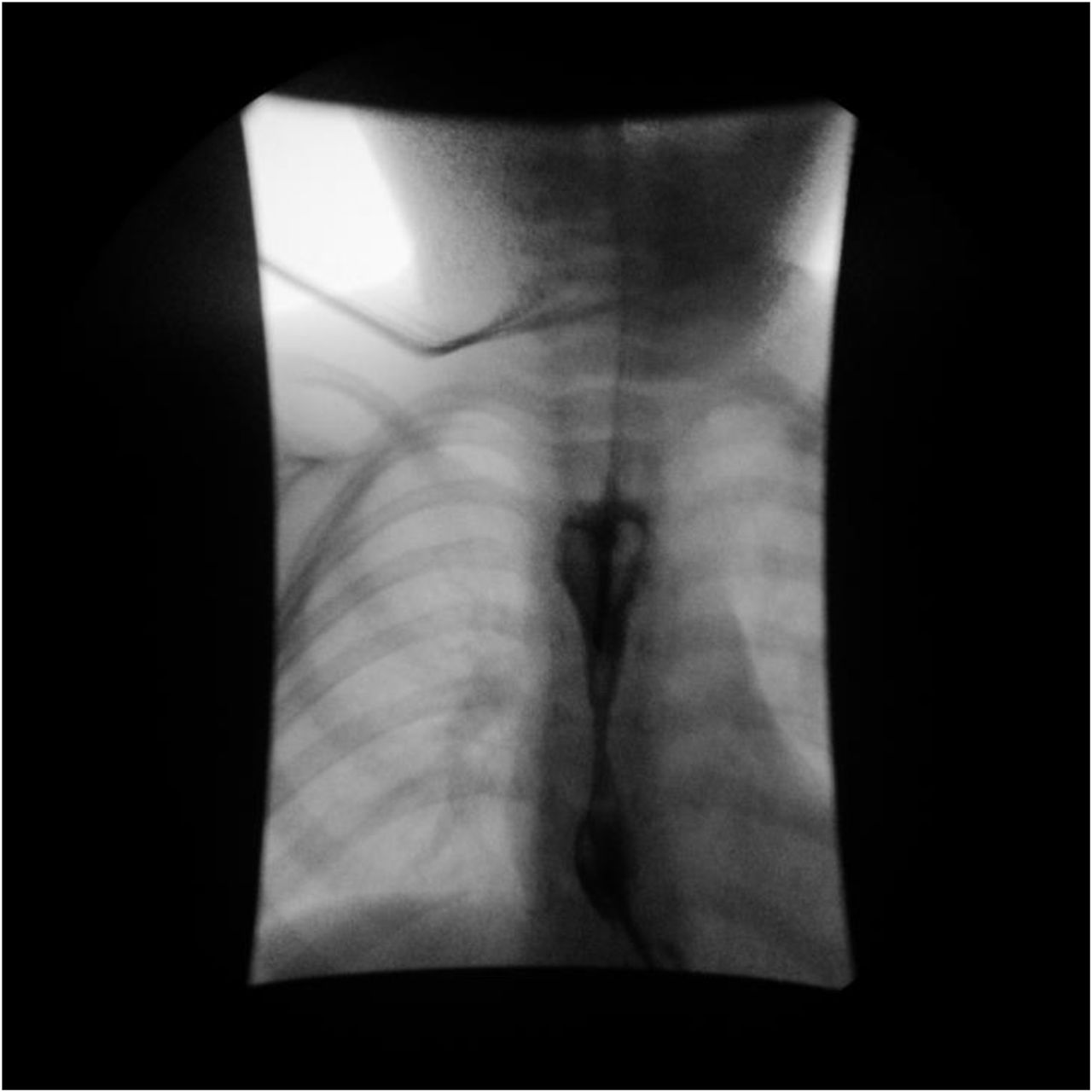 Figure 3. Esophagram obtained in a 3-year-old male patient demonstrates smooth tapering of the distal esophagus at the T7-8 level, which is compatible with esophageal stricture. The smooth appearance without any areas of mucosal irregularity or ulceration suggests a congenital etiology or prior caustic esophageal injury. An enteric tube was used to introduce contrast material, as the patient refused to drink it. Pathology revealed esophagitis with basal cell hyperplasia, >36 eosinophils per high-powered field, subepithelial fibrosis, and papillary sclerosis. The patient was diagnosed with EoE, and budesonide slurry was started.
Figure 3. Esophagram obtained in a 3-year-old male patient demonstrates smooth tapering of the distal esophagus at the T7-8 level, which is compatible with esophageal stricture. The smooth appearance without any areas of mucosal irregularity or ulceration suggests a congenital etiology or prior caustic esophageal injury. An enteric tube was used to introduce contrast material, as the patient refused to drink it. Pathology revealed esophagitis with basal cell hyperplasia, >36 eosinophils per high-powered field, subepithelial fibrosis, and papillary sclerosis. The patient was diagnosed with EoE, and budesonide slurry was started.
From Zucker EL, Nagendra G, Bhardwaj V. A 3-year-old male with unusual esophageal stricture. Pediatrics. 2020;146:471-472.
One grading system, the Endoscopic Reference Score (EREFS), has been modified and validated for use even with nonexpert endoscopists. See the Clinical Tools section for the EREFS tool.
Rarely, a child with EoE will not have abnormal findings at endoscopy. A lack of abnormal endoscopic findings does not rule out EoE as a diagnosis. Eosinophilia may still be present, and a biopsy should be performed even in the absence of typical endoscopic findings of EoE.
Tissue samples should always be obtained during endoscopy because histologic examination of the samples is required for diagnosis and for treatment follow up. Samples should be obtained from at least 5 different areas of the esophagus (proximal and distal).
Repeat endoscopic biopsy is often necessary to assess inflammation and guide treatment options. Although symptoms in children can correlate with histological findings and outcomes, a child’s symptoms alone may not be sufficient to provide adequate information for management. There is currently no standardized method to guide long-term monitoring (ie, frequency of endoscopy or follow-up evaluation). Long term follow up should be tailored for each patient.
Less invasive options for upper endoscopy
Upper endoscopy in children requires general anesthesia. Given the need for repeat biopsy to histologically assess treatment outcomes, less invasive options have been explored. These options may be considered for assessing treatment outcomes in specific situations:
- Esophageal string test (EST) – a capsule technology that captures eosinophil-related proteins
- Cytosponge – originally designed to assess esophageal mucosa in Barrett esophagus
- Transnasal endoscopy – sedation is not necessary to assess esophageal inflammation and obtain biopsy
- Tethered confocal microscopy capsule – use of this tool has been assessed in adults but has not been extrapolated for use with children at the time of this publication
Diagnostic Criteria
A diagnosis of EoE can be established in the presence of clinical symptoms of EoE and intraepithelial eosinophilia (≥15 eosinophils/hpf) restricted to the esophagus.
- The presence of other atopic disease increases the clinical suspicion for EoE.
- EoE is diagnosed only in the absence of other causes of esophageal eosinophilia.
- Eosinophilia that is identified in other areas of the upper or lower gastrointestinal tract, is not consistent with a diagnosis of EoE, and other diagnoses should be considered.
Although current guidelines require intraepithelial eosinophilia (≥15 eosinophils/hpf) for diagnosis, a validated histologic EoE scoring system (EoEHSS) takes into consideration inflammatory features apart from intraepithelial eosinophil quantitation and may correlate more strongly with treatment outcomes than eosinophil counts alone. These histologic features include:
- Eosinophil abscess
- Eosinophil surface layering
- Basal zone hyperplasia
- Dilated Intercellular spaces
Before a diagnostic biopsy is performed (but not before biopsy to monitor treatment response), withdrawing proton pump inhibitor medication for at least 3 weeks prior is advised.
Diagnosis is complicated by the fact that EoE has at least 3 subtypes that do not reliably induce increased numbers of eosinophils and may not qualify for a classical EoE diagnosis.
Differential Diagnosis
EoE can present in a wide variety of clinical scenarios. Care must be taken to rule out causes of eosinophilia aside from EoE (below) and to investigate the presence of conditions that mimic the clinical picture of EoE.
Conditions That Can Mimic EoE
When to Refer
Any child with suspected EoE requires an evaluation by a gastroenterologist because endoscopy and biopsy are required to establish a diagnosis. In addition, allergist/immunologists are often involved in the care of children with EoE, particularly when the children have comorbid allergic conditions. When available, gastroenterologists and allergist/immunologists have the expertise and resources available to help guide management decisions and monitoring for EoE, although the primary care pediatrician remains a vital part of each patient’s medical home.
Refer a family to a dietitian when an elimination diet is implemented. If this is not feasible, then refer a patient to a dietitian when a patient on an elimination diet experiences the following:
- Weight loss (or excessive weight gain)
- Inadequate growth
- Treatment failure caused by inadequate or suspected lack of dietary adherence
- Diet of poor nutritional quality
- Social isolation related to diet
- Low level of social support or limited access to substitute foods
Refer to a dedicated EoE clinic:
- When available; these multispecialty clinics can offer expertise and comprehensive care from the time of establishing diagnosis of EoE through long term management
- When remission fails to occur after first-line therapy options are explored (PPI, dietary changes, swallowed topical steroids)
Refer to an eating disorder specialist:
- In the presence of food refusal, aversions, or restrictions that result in
- Weight loss
- Nutritional deficiencies
- Evidence of body shape or weight concerns

The development of this information was made possible through support from Sanofi and Regeneron.
Last Updated
06/13/2023
Source
American Academy of Pediatrics