EoE is a chronic disease that requires long-term treatment. The goals of treatment are to:
- Decrease eosinophilic inflammation
- Alleviate symptoms
- Prevent disease progression
- Prevent disease complications (malnutrition, suboptimal growth))
- Support normal development and psychological adjustment
Treating children with EoE involves diet therapy and/or medical therapy. Children with strictures and food impaction that do not improve with medical and/or diet therapy may require dilation.
A multi-center, retrospective study drawing from a European database of patients with EoE (adults and children) demonstrated that clinical and histologic remission or response occurred in 82% of patients taking topical steroids, 69% of patients taking proton pump inhibitors, and 42% of patients on empirical elimination diets.
The choice of treatment depends on the clinical picture, as well as family circumstance and preferences.
- EoE is a condition that is highly variable in its presentation, severity and response to treatment. As such, each patient and family should participate in a shared decision-making discussion so they fully understand risks, benefits and expected outcomes associated with all treatment options.
- Recent guidelines promote shared decision making and individualized approaches towards management. For example, one patient/family may place high value on not restricting their diet as much as possible whereas another may wish to avoid medications.
Dietary Therapy
For many children, EoE is a non-IgE-mediated allergic disease, thus removal of relevant food allergens can cause remission of the disease.
- It is important to acknowledge that elimination diets can be difficult to adhere to and can decrease quality of life and possibly promote disordered eating.
- Early research demonstrated highest rates of remission with complete elemental diets followed by six-food elimination diets (see below) but these are also often unsustainable for long periods of time.
- Early research also evaluated the use of IgE skin prick or serologic tests to guide specific food elimination diets, but this is now considered outdated due to false positive results and inconsistency in identification of food triggers.
Dietary therapy has 3 main approaches:
- Elemental diet
- Empirical food elimination (four or six-food elimination)
- Milk elimination
Medical Therapy
Dilation
When dietary or anti-inflammatory treatment are ineffective, children with EoE may develop esophageal strictures or stenosis. In some children, esophageal dilation may be necessary to prevent food impaction and pain.
- One retrospective study of 451 pediatric dilations showed that esophageal dilation has a low rate of serious adverse events that necessitate medical intervention (3%); chest pain was reported in approximately 15% of children.
- Some strictures form in very young children with EoE. The youngest documented age at which stricture formation requiring dilation occurred in a child was 3 years (Figure 4).
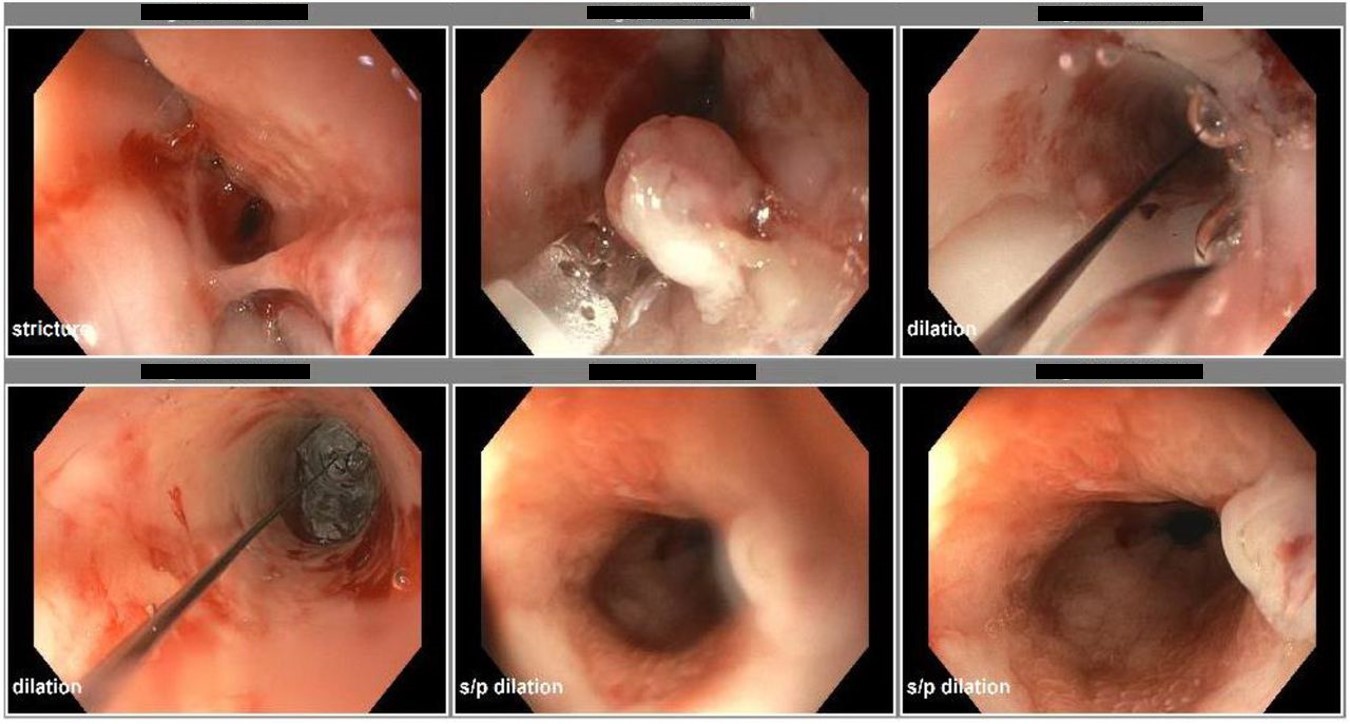
Figure 4. In the same 3-year-old male patient as in Figure 3, endoscopic findings show the sequence of distal esophageal stricture pre-dilation, intra-dilation with water-filled balloon dilator from 5 mm to 10 mm with safe degree of wall blanching seen through the dilating balloon, and post-dilation following removal of the balloon dilator.
From Zucker EL, Nagendra G, Bhardwaj V. A 3-year-old male with unusual esophageal stricture. Pediatrics. 2020;146:471-472.

The development of this information was made possible through support from Sanofi and Regeneron.
Last Updated
06/12/2023
Source
American Academy of Pediatrics