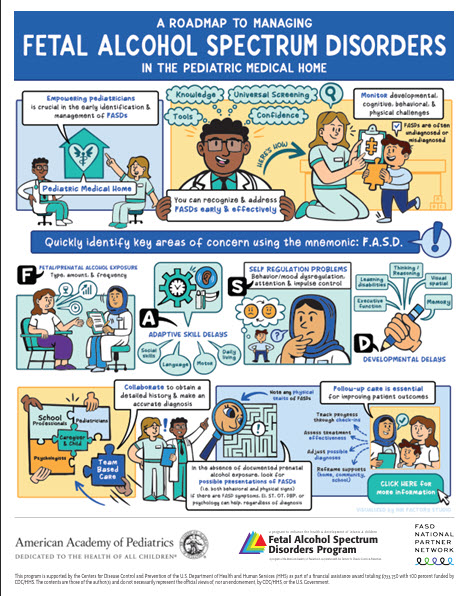
A Roadmap to Managing FASDs in the Pediatric Medical Home
A practical guide to help pediatricians navigate the identification of children with fetal alcohol spectrum disorders (FASDs) within the medical home. This job aid outlines key steps, decision points, and resources to support coordinated, family-centered care.
Familiarity with diagnostic approaches for FASDs contributes to accurate diagnosis, treatment, and care for children with FASDs and their families. Physicians can consider the diagnosis of an FASD when they recognize and assess one or more of the following factors or symptoms of a child
- History of prenatal alcohol or substance exposure
- Developmental, cognitive, or behavioral concerns
- Complex medical concerns (e.g. cardiac)
- Intrauterine or postnatal growth deficits (e.g. microcephaly)
- Cardinal dysmorphic facial characteristics associated with FAS are present
- History of a sibling diagnosed with an FASD
Differential diagnosis of any of the above concerns should include an evaluation for an FASD. Investigation would involve screening for physical characteristics (growth, facial dysmorphology), neurodevelopmental screening, and a sensitive exploration of a history for possible prenatal alcohol exposure.
Pediatricians can choose which diagnostic scheme to use to make an FASD diagnosis. Below is a list of some of the diagnostic schema.
Approach: Neurobehavioral Disorder Associated With Prenatal Alcohol Exposure
Description: This system focuses on neurodevelopmental impairments associated with prenatal alcohol exposure with three general areas of greatest risk identified:
1) neurocognition, 2) self-regulation, and 3) adaptive impairment. The DSM-5 Taskforce developed clinical mental health criteria to recognize Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (N D-PAE).
The ND-PAE diagnosis requires evidence of more than minimal prenatal alcohol exposure. Although ND-PAE is included as a condition in Section 111 of DSM-5 (conditions for further study), the diagnosis and associated mental health codes can be used. ND-PAE can also be used as a specifier for children diagnosed with Intellectual Disability. Finally, the ND-PAE diagnosis can co-occur with other FAS Ds with physical features such as FAS or PFAS.
Approach: Updated Clinical Guidelines for Diagnosing Fetal Alcohol Spectrum Disorders
Description: These updated guidelines are available in the research literature and follow the 1996 Institute of Medicine (IOM) framework. Diagnoses and criteria included in this system are: Fetal Alcohol Syndrome (FAS), Partial Fetal Alcohol Syndrome (PFAS), Alcohol-Related Neurodevelopmental Disorder (ARND) and Alcohol-Related Birth Defects (ARBD).
Approach: FASD 4-Digit Diagnostic CodeTM, Third Edition
Description: The four digits in the code reflect the magnitude of expression of the key diagnostic features of an FASD: (1) growth deficiency, (2) facial features, (3) neurocognitive structural and functional abnormalities, and (4) prenatal alcohol exposure.
For each domain of assessment (i.e., exposure, neurodevelopment, dysmorphia & growth) the severity of exposure or impact is rated on a four-point scale. These individual domain rankings are combined into a "4-Digit-Code". The codes are then converted to a diagnostic label provided in a comprehensive table. An additional diagnostic category used in this system is Static Encephalopathy.
Approach: Fetal Alcohol Spectrum Disorder: A Guideline for Diagnosis Across the Lifespan (Cook et al, CMAJ, 2015)
Description: This diagnostic process consists of a physical examination, the creation of a differential diagnosis, a neurobehavioral assessment, treatment, and follow-up. The diagnosis requires a multidisciplinary approach that leads to diagnoses of an FASD with or without cardinal dysmorphic facial features.
In this Canadian system, unlike in US systems, the term FASD is used as a clinical diagnosis. This system does not include growth restrictions as criteria, although clinicians are urged to assess and note any growth issues. This system also includes an "at risk" category for children who present with issues related to prenatal alcohol exposure but not meet criteria for an FASD diagnosis.
The AAP recommends that the child’s pediatrician assess for prenatal alcohol exposure and considers an FASD in their differential diagnosis. Children who have symptoms that are consistent with an FASD may benefit from having a comprehensive assessment for an FASD by a multidisciplinary team. It is not expected for a primary care provider to make an FASD diagnosis in isolation. Primary care providers should keep an FASD in their differential diagnosis and make appropriate referrals for diagnosis and co-management.
Last Updated
07/17/2025
Source
American Academy of Pediatrics