Overview
Pediatricians and other healthcare professionals can play an important role for children and adolescents diagnosed with an FASD through family-centered care that promotes and supports healthy families. Effective partnerships with families require affirmative language, guidance to accurate and timely information, access to community resources, interventions and support services.
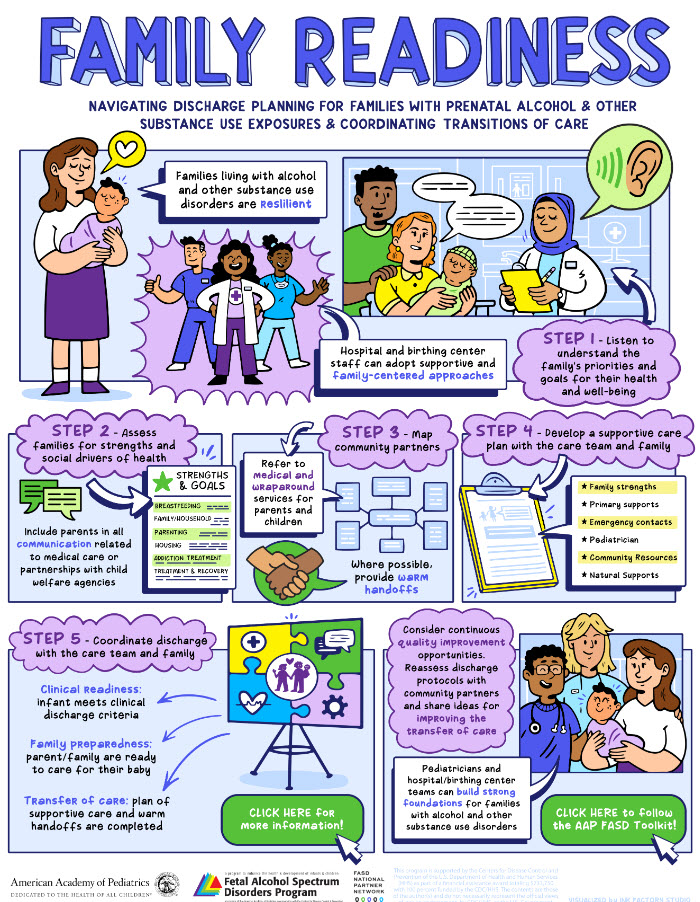
Step 1 - Listen to understand the family’s priorities and goals for their health and well-being
Compassionate non-judgmental routine screening is crucial for all pregnant and postpartum patients, regardless of any history of substance use. Offering integrated, personalized services—such as lactation support and family-focused assistance—can help address specific needs. An initial step in identifying harmful substance use is universal screening. The Screening, Brief Intervention, and Referral to Treatment (SBIRT) model, an effective approach based on motivational interviewing principles, can be used to discuss alcohol and other substance-related issues with pregnant persons.
This initial step is also crucial in building a foundation of trust and understanding. This can help reduce bias and stigma associated with substance use. Assumptions, stereotypes, and biases about individuals who consume alcohol while pregnant may lead to unjust or prejudicial treatment of the individual. One cannot assume they know or understand why a person drinks alcohol during pregnancy. For instance, some individuals don’t know they are pregnant; are not aware that alcohol in any amount may be harmful to their developing fetus; or may have an alcohol use disorder. Evidence suggests that greater provider knowledge about alcohol and substance use disorders (SUD) helps reduce stigmatization and improves health outcomes for patients.
Tips For Maintaining Open and Non-Judgmental Conversations
- Let parents and caregivers know that you ask all patients these questions.
- Begin by inquiring about general topics related to pregnancy and then move toward more specific questions about prenatal substance exposures.
- Show compassion by asking questions and actively listening.
- Use person-first language (e.g., “parent with a substance use disorder”).
- Stick to factual information.
- Remind parents and caregivers that you care about their well-being as well as that of their child.
- Don’t be afraid to ask about recovery.
- Practice universal screening. Your patients will be as comfortable answering your questions as you are asking them.
Step 2- Assess families for strengths and social drivers of health.
Including parents in all communication related to medical care and partnerships with child welfare agencies ensures that their voices are heard and respected. Hospital and birth center staff can encourage families to seek advocates to ensure that family voices are heard. Identifying and addressing potential risk factors, such as parenting classes or financial assistance, can assist families in establishing effective support networks. By fostering a collaborative approach and connecting families with resources, hospital and birth center staff can help families feel more secure and supported, ultimately leading to better outcomes for children and parents.
Step 3- Map community partners
Pregnant persons with alcohol and/or substance use during pregnancy require comprehensive care that goes beyond addressing their immediate medical and newborn needs. Holistic approaches aim to recognize that alcohol and/or substance use impacts various aspects of an individual’s life, addressing mental health, social support, parenting, and recovery simultaneously. Encourage self-care by connecting them with resources—family, friends, social workers, home visitors and professionals in their health care journey—OBGYN, family physician, or their child’s pediatrician. Remind them that they’re not alone, and seeking help is both normal and essential.
Key Term: Warm hand-offs—where one provider directly introduces the patient to another—facilitate continuity of care.
Step 4- Develop a supportive care plan with the care team and family
For postpartum patients and newborns with prenatal alcohol exposure, hospital and birth center staff play a role as advocates and partners, ensuring that essential services are available from the outset. When working with families affected by alcohol and/or substance use, a patient- and family-centered approach is a critical element of an integrated care model. To ensure seamless transitions, offer care coordination in collaboration with members of a diverse interdisciplinary care team that includes patients, families, caregivers, nurses, physicians, social workers, care navigators, early intervention providers, school professionals, and staff from Title V Maternal and Child Health programs. Additionally, hospital and birthing center staff can suggest resources that were identified during the parents’ postpartum care. Communicating with the family’s chosen pediatrician can help ensure comprehensive and continuous care for postpartum patients and newborns with prenatal substance exposure.
Communicating with family physicians for long-term care
Family physicians provide care across the lifespan and often have an established relationship with a patient prior to pregnancy. Through continuity of care that reduces fragmentation and improves patient safety and quality of care, family physicians gain the confidence and trust of patients, which allows them to be effective patient advocates. Whether a patient sees their family physician for their obstetrical care or reestablishes the relationship post-pregnancy, a family physician working with an interdisciplinary team can use existing and prior knowledge of the patient and their needs to make timely adjustments, especially as those needs change. Family physicians can connect patients with necessary resources and monitor progress through regular visits.
Step 5- Coordinate discharge with the care team and family
Amid the joys of the newborn phase, parents also struggle with the demands of caring for their infants. It’s normal for them to feel frustrated and exhausted. Providing guidance on common difficulties, such as soothing a crying baby and managing sleep patterns, can significantly ease their parenting journey. When providing discharge instructions, it is essential also to include comprehensive guidance on various aspects of postnatal care that include addressing substance use and lactation. For instance, you can emphasize the benefits of breastfeeding for both the parent and the baby and provide resources for support if the parent is struggling with substance use. Providing immediate referrals and contact information for local support groups, hotlines, and healthcare providers can be invaluable for those needing assistance, ensuring clinical readiness and family preparedness.
Key Tool: HealthyChildren.org, created by the American Academy of Pediatrics (AAP), provides trustworthy information and resources on child health, as well as parenting tips.
Lastly, hospital and birth center staff can explore continuous quality improvement opportunities by reassessing discharge protocols in collaboration with community partners and sharing ideas to enhance the transfer of care. Pediatricians and hospital birth center teams can play a pivotal role in establishing strong foundations for families dealing with alcohol and other substance use disorders.
Resources
Hospital and birthing center staff have access to several valuable national resources to support families impacted by prenatal alcohol and other substance exposure:
AAP Fetal Alcohol Spectrum Disorders (FASD) Toolkit
- A comprehensive resource designed to help healthcare professionals raise awareness, promote screening, and ensure timely interventions for children affected by FASDs.
- Fetal Alcohol Spectrum Disorders: Recognition and Management, a free online course.
AAFP Resources to Address Alcohol and Other Substance Use
- Practice Manual: A comprehensive guide designed to help family physicians address patients’ use of alcohol and other substances, including during pregnancy.
- Addressing Prenatal Alcohol and Other Substance Use, a free online course:
- The American College of Obstetricians and Gynecologists (ACOG) guide emphasizes that no amount of alcohol is safe during pregnancy, as it can lead to serious health risks for the baby.
FASD United
- Recovering Mothers Anonymous: a 12-step program for mothers who gave birth to a child exposed to alcohol.
- FASD Family Navigator Program: peer support and warm handoff with no referral required to community resources that are FASD- or prenatal alcohol and other substances-informed (www.fasdunited.org/family-navigator or dial 202-785-4585)
Family Voices
- A national, non-profit, family led organization focused on promoting quality health care for all children and youth, particularly those with special healthcare needs.
Family-to-Family Health Information Centers (F2F HICs)
- Non-profit organizations that help families of children and youth with special healthcare needs and the professionals who serve them. F2F HICs are typically staffed by parents of children and youth with special healthcare needs.
National Center on Substance Abuse and Child Welfare (NCSACW)
- Offers resources related to Plans of Safe Care, child welfare, and maternal mental health.
Parent to Parent USA
- A grassroots organization that offers guidance to families of children and youth with special healthcare needs through peer support.
Social services and Other Assistance
- 2-1-1 is a 3-digit number that provides information and referrals to food, housing, mental health, social services and other assistance (Dial 211).
Substance Abuse and Mental Health Services Administration (SAMHSA)
- Provides clinical guidance for treating pregnant persons with alcohol and other substance use, as well as mental health services.
Last Updated
07/02/2025
Source
American Academy of Pediatrics