Pediatric care coordination is a patient- and family-centered, assessment-driven, team-based activity designed to meet the needs of children and youth while enhancing the caregiving capabilities of families and other caregivers. Care coordination and case management reach across medical and nonmedical domains to address interrelated medical, social, developmental, behavioral, educational, and financial needs to achieve optimal health and wellness outcomes. Care coordination and case management are essential components of the services provided by members of the patient/family-centered medical home team.
Facilitation of Community-based Services
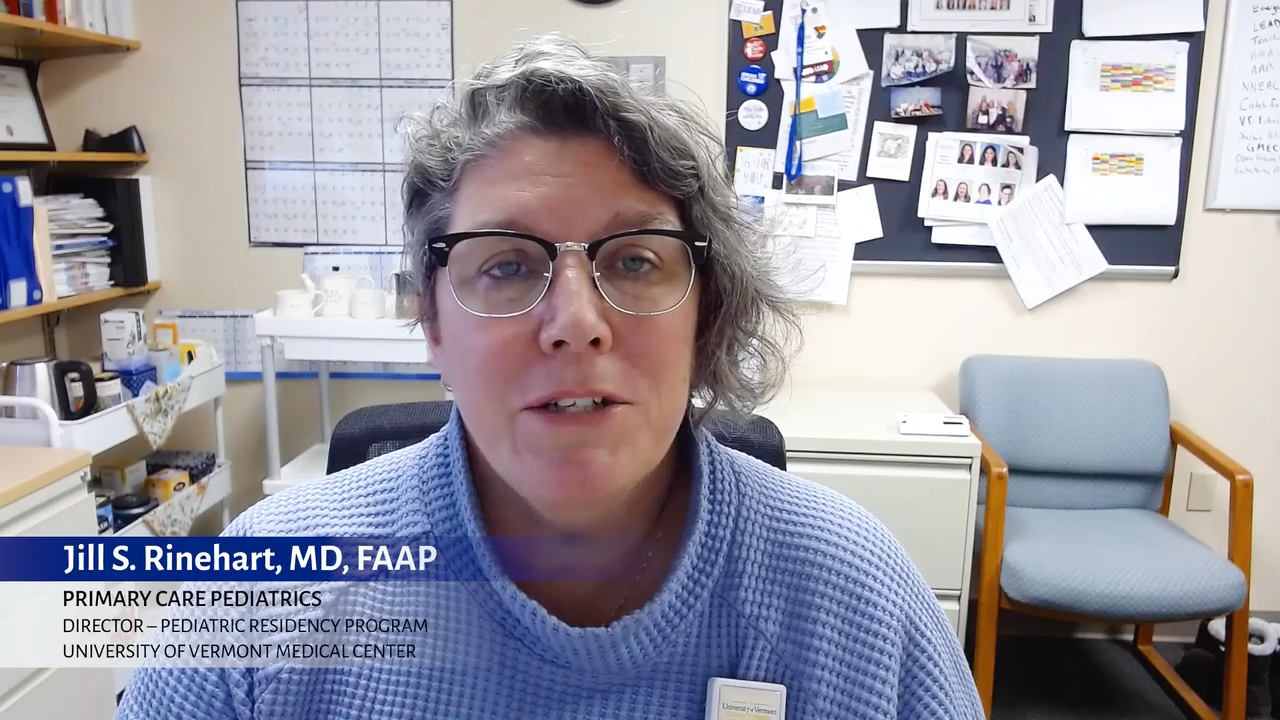
Pediatricians can accompany families in their health journey by facilitating access to community-based resources that support children and families with an FASD. View this video or download a free one-page resource to learn more.
Care Coordination through a Patient- and Family-centered Medical Home
For children and youth with prenatal alcohol exposure, including those with significant social determinant of health risk factors, a patient- and family-centered medical home is a critical element of an integrated care model, offering care coordination in collaboration with the members of a diverse care team, across settings. This diverse care team includes patients, families, caregivers, nurses, physicians, social workers, community health workers, care managers, care navigators, case managers, early intervention providers, education professionals, and staff from Title V Maternal and Child Health programs.
Effective case management and care coordination begins with recognition that an FASD is a type of permanent brain injury that has no cure and that an individual’s presentation depends upon personal genetics, amount and frequency of exposure to prenatal alcohol use during gestation, and other factors. While there is no cure for an FASD, lifelong case management, using targeted behavioral and pharmacologic interventions, can mitigate symptoms and is an essential resource for most individuals. To be most effective, this may require care transitions as an individual with an FASD at several developmental stages. FASDs manifest differently across the lifespan and intervention and treatment strategies that were effective at a specific developmental stage may not be effective during a different developmental stage.
Pediatric Care Coordination Curriculum: An Interprofessional Resource to Effectively Engage Patients and Families Achieving Optimal Health Outcomes, 2nd Edition
The Pediatric Care Coordination Curriculum was designed to emphasize the central role of families, caregivers, children, youth, and young adults in collaboration with a multidisciplinary group of care team members. It identifies a framework for integrating efforts across time, settings, and disciplines. The curriculum aims to build the capacity of the multidisciplinary care team and families through effective implementation of key components of care coordination, constructive and collaborative communication within interprofessional care teams and families, and investment in technology solutions (Boston Children’s Hospital).
Achieving a Shared Plan of Care with Children and Youth with Special Health Care Needs
Identifying, accessing, and coordinating services that benefit an individual child or youth with special health care needs is a difficult but necessary part of good quality health care. Providing such care requires a continuous collaborative effort by children/youth, families, and their care team. The best means of guiding and documenting these efforts is an individualized and comprehensive shared plan of care.
An individualized and shared plan of care includes the information necessary to ensure that issues affecting a child’s health and health care are identified, and that activities and accountability for addressing them are documented. The best strategies, care structures, processes and outcomes result when patients, families, and health care providers form trusting, caring partnerships and draw upon one another’s perspectives and expertise.
Patients and families should be part of the goal setting and creating, implementing, and updating of a formal, written plan of care that is sensitive to their language, values, and culture. Linking families with other families/caregivers with shared experiences can be very helpful in diagnosis and long-term support for families.
AAP Policy
Additional Information
Care Coordination Resources (aap.org)
Care Coordination and Referral: Partnering with the Community (video)
FASD United (formerly National Organization on Fetal Alcohol Syndrome (NOFAS)
Last Updated
12/03/2024
Source
American Academy of Pediatrics