For the best health outcomes, the American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for approximately 6 months followed by continued breastfeeding with complementary foods for at least 2 years and beyond as mutually desired.
The AAP provides detailed information on breastfeeding and breastfeeding support for clinicians here.
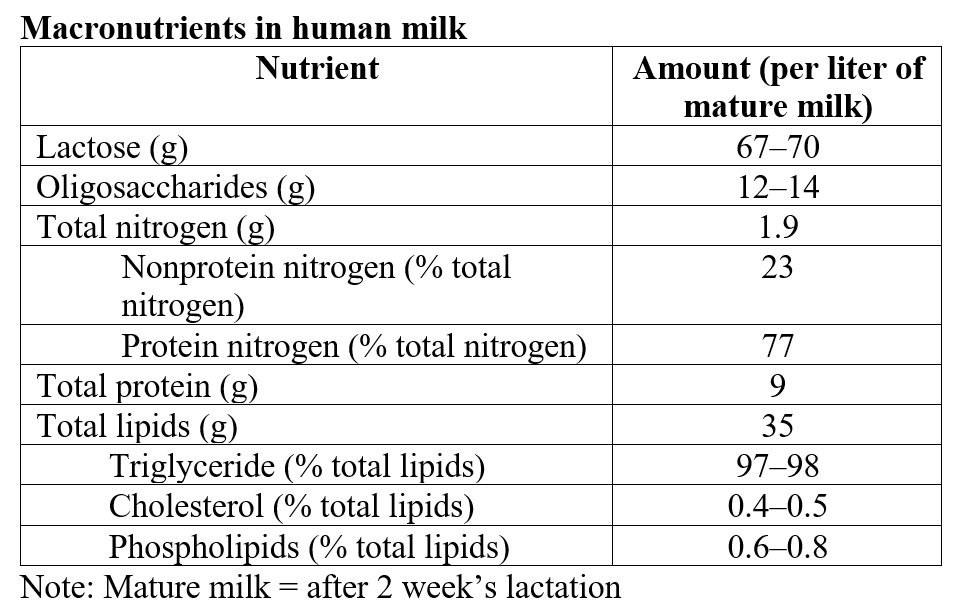
Components of Human Milk
Human milk contains:
- macronutrients and micronutrients
- active biological components, including
- immunoglobulins
- cytokines
- growth factors
- hormones
- antimicrobial agents
- immune cells
- stem cells
- prebiotic oligosaccharides
- Probiotic bacteria
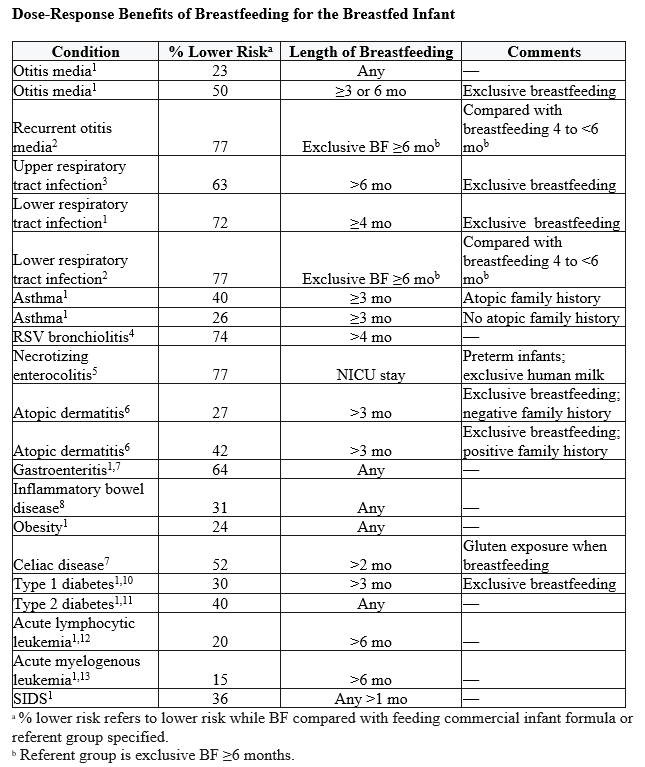
The Benefits of Breastfeeding
In addition to benefitting infants [link to “Dose response” table below], breastfeeding offers
- societal benefits
- environmental, in that it doesn’t require manufacturing (which uses energy and produces waste and pollution)
- parents miss less work because breastfed babies are not sick as often
- maternal benefits
- reduced risk for excessive bleeding during menstruation
- reduced risk for several diseases such as
- rheumatoid arthritis
- hypertension
- type 2 diabetes
- certain cancers
References:
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep). 2007 Apr;(153):1-186. [link]
- Chantry CJ, Howard CR, Auinger P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics. 2006 Feb;117(2):425-32. [link]
- Duijts L, Jaddoe VW, Hofman A, Moll HA. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics. 2010 Jul;126(1):e18-25.
[link] - Nishimura T, Suzue J, Kaji H. Breastfeeding reduces the severity of respiratory syncytial virus infection among young infants: a multi-center prospective study. Pediatr Int. 2009 Dec;51(6):812-6. [link]
- Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawöger R, Kiechl-Kohlendorfer U, Chan GM, Blanco CL, Abrams S, Cotten CM, Laroia N, Ehrenkranz RA, Dudell G, Cristofalo EA, Meier P, Lee ML, Rechtman DJ, Lucas A. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr. 2010 Apr;156(4):562-7.e1. [link]
- Zutavern A, Brockow I, Schaaf B, Bolte G, von Berg A, Diez U, Borte M, Herbarth O, Wichmann HE, Heinrich J; LISA Study Group. Timing of solid food introduction in relation to atopic dermatitis and atopic sensitization: results from a prospective birth cohort study. Pediatrics. 2006 Feb;117(2):401-11. [link]
- Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeed Med. 2009 Oct;4 Suppl 1:S17-30. [link]
- Barclay AR, Russell RK, Wilson ML, Gilmour WH, Satsangi J, Wilson DC. Systematic review: the role of breastfeeding in the development of pediatric inflammatory bowel disease. J Pediatr. 2009 Sep;155(3):421-6. [link]
- Akobeng AK, Ramanan AV, Buchan I, Heller RF. Effect of breast feeding on risk of coeliac disease: a systematic review and meta-analysis of observational studies. Arch Dis Child. 2006 Jan;91(1):39-43. [link]
- Rosenbauer J, Herzig P, Giani G. Early infant feeding and risk of type 1 diabetes mellitus-a nationwide population-based case-control study in pre-school children. Diabetes Metab Res Rev. 2008 Mar-Apr;24(3):211-22. [link]
- Das UN. Breastfeeding prevents type 2 diabetes mellitus: but, how and why? Am J Clin Nutr. 2007 May;85(5):1436-7. [link]
- Kwan ML, Buffler PA, Abrams B, Kiley VA. Breastfeeding and the risk of childhood leukemia: a meta-analysis. Public Health Rep. 2004 Nov-Dec;119(6):521-35. [link]
- Rudant J, Orsi L, Menegaux F, Petit A, Baruchel A, Bertrand Y, Lambilliotte A, Robert A, Michel G, Margueritte G, Tandonnet J, Mechinaud F, Bordigoni P, Hémon D, Clavel J. Childhood acute leukemia, early common infections, and allergy: The ESCALE Study. Am J Epidemiol. 2010 Nov 1;172(9):1015-27. [link]
Breastfeeding the Newborn
National efforts to promote breastfeeding have driven improvements in breastfeeding initiation rates. The US national average for breastfeeding initiation is approximately 84%.(ref) However:
- by 3 months only 47% of mothers are exclusively breastfeeding and this rate drops to 25% at 6 months.
- Of babies born in 2019, approximately 1 in 6 did not receive any breastmilk (ref)
- Breastfeeding initiation rates are generally higher among infants of Asian and White mothers and lower among Black mothers and AI/AN, though this is not true in all states.
- Breastfeeding disparities are often state-specific
- Check updated breastfeeding data by state at the CDCs interactive trend map
Pediatrician’s Role in Breastfeeding
The pediatrician’s role in breastfeeding initiation is critical. Pediatricians should:
- Promote breastfeeding as the norm for infant feeding
- Recommend exclusive breastfeeding for approximately 6 months.
- Encourage continuing breastfeeding until at least 12 months of age.
- Add complementary foods at approximately 6 months of age.
- Educate parents about the importance of human milk for all infants.
- Human milk and its components.
- Benefits of breastfeeding.
- Correct any false beliefs about infant feeding.
- Prepare mother for hospital experience and recommend that:
- Baby goes skin-to-skin at delivery
- Routine nursery care and preventive treatments such as neonatal eye prophylaxis
- and vitamin K should be administered, but can be delayed up to 6 hours to allow
- for first nursing
- 24-hour rooming-in is practiced
- Elective procedures (eg, bathing, circumcision) are delayed until infant is feeding well
- Encourage unrestricted nursing.
- Baby should nurse whenever interested (8–12 times per day).
- Educate parents about norms in baby feeding, weight, stooling, and voiding.
- Avoid unnecessary supplements or pacifiers until breastfeeding is well established.
- Address parental questions and concerns.
- Avoid any promotion of commercial infant formula or feeding equipment in the hospital or office.
- Implement breastfeeding-supportive office practices.
Establish office practices that support breastfeeding
- Have a written breastfeeding-friendly office policy.
- Train staff in breastfeeding support skills.
- Discuss breastfeeding during prenatal visits and at each well-child visit.
- Encourage exclusive breastfeeding for 6 months.
- Provide appropriate anticipatory guidance that supports the continuation of breastfeeding as long as desired.
- Incorporate breastfeeding observation into routine care.
- Educate mothers on breast milk expression and return to work.
- Provide noncommercial breastfeeding educational resources for parents.
- Encourage breastfeeding in the waiting room but provide private space on request.
- Eliminate the distribution of free formula.
- Train staff to follow telephone triage protocols to address breastfeeding concerns.
- Collaborate with the local hospital or birthing center and obstetric community regarding breastfeeding care.
- Link with breastfeeding community resources.
- Monitor breastfeeding rates in your practice.
Managing Conditions Often Associated with Breastfeeding
Hypoglycemia
Hypoglycemia in breastfed infants is a commonly cited concern among physicians
- Healthy full-term infants with normal feeding patterns have adaptions to prevent problematic hypoglycemia.
- Infants most at risk are small or large for gestational age, late preterm, or born to diabetic mothers
- Reducing the occurrence of hypoglycemia can be facilitated by
- Encouraging skin-to-skin care
- Improving milk intake by early and frequent breastfeeding
- AAP recommends screening for hypoglycemia in symptomatic or at-risk infants only.
- Routine supplementation of healthy, asymptomatic breastfed infants to prevent hypoglycemia is not indicated.
- Manage mild hypoglycemia with prompt feeding
Breastfeeding Jaundice
- Newborns who are not feeding well are at risk of breastfeeding jaundice, sometimes called suboptimal intake jaundice
Usually occurs in the first week of life
- low milk intake, relative dehydration, delayed passage of bilirubin-rich meconium, and an active enterohepatic circulation of bile may lead elevated bilirubin.
- Infants with increased rates of bilirubin production caused by hemolytic processes (eg, ABO incompatibility, glucose-6-phosphate dehydrogenase [G6PD] deficiency), bruising, or ingested maternal blood may be at increased risk
- infants with immaturities in conjugating bilirubin (typically seen in Asian or late preterm infants or those with Gilbert syndrome) may also have jaundice in the early days after birth
- Prevention of breastfeeding jaundice is key.
- Encourage exclusive and frequent breastfeeding at least 8 to 12 times per day, avoid water or unnecessary formula supplements, and teach mothers proper latch technique to help prevent poor intake, excessive weight loss, and jaundice
- There is never a need to interrupt breastfeeding
- an appropriate response is to optimize intake by improving milk transfer, by having the mother express milk to increase milk intake, or with the judicious use of pasteurized donor milk or formula supplements for infants with significant hyperbilirubinemia
- supplementation is not routinely indicated.
Breast Milk Jaundice
Jaundice that occurs in healthy thriving breastfed infants usually beyond the 2nd week of life is known as breast milk jaundice (BMJ).
- In BMJ, serum unconjugated bilirubin remains elevated, and a few infants may have elevated concentrations for as long as 6 to 12 weeks
- by week 3, two-thirds of healthy, thriving breastfed infants have serum bilirubin concentrations above 1.5 mg/dL, and 30% are clinically jaundiced.
- in contrast, formula fed infants serum bilirubin declines to less than 1.5 mg/dL by day 11 or 12 after birth
- This elevation in serum bilirubin is a normal response to breastfeeding, and
other than the presence of jaundice, infants with BMJ seem healthy - The cause of breast milk jaundice is unknown, but factors in human milk that increase the enterohepatic cycle of bilirubin or genetic variations that impair bilirubin hepatic conjugation may play a role.
Breastfeeding should be continued, and in most cases the parent or parents should be reassured.
Last Updated
05/31/2022
Source
American Academy of Pediatrics