Coding of evaluation and management (E/M) services continues to be the most asked-about coding topic on the coding and payment hotline. Medical Decision Making (MDM) and total time concepts have been applied to the majority of E/M code sets. Understanding how to apply CPT guidelines to code selection will help you to write meaningful documentation that will support both the medical necessity of the service you provide and the CPT codes you report for payment.
Medical Decision Making
MDM is the process of evaluating the complexity of a problem or condition, the amount and/or complexity of data to be reviewed and analyzed, and the risk of complications of patient management.
Components of MDM:
- Number and complexity of problem(s) that are addressed during the encounter
- Amount and/or Complexity of Data to Be Reviewed and Analyzed
- Risk of Complications and/or Morbidity or Mortality of Patient Management
Levels of MDM:
- Straightforward
- Low
- Moderate
- High
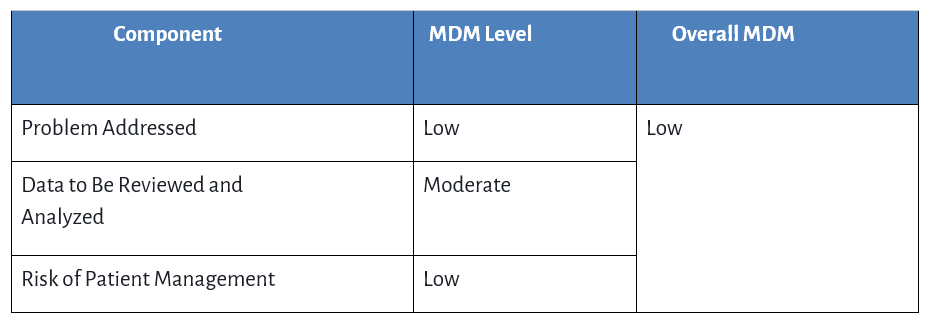
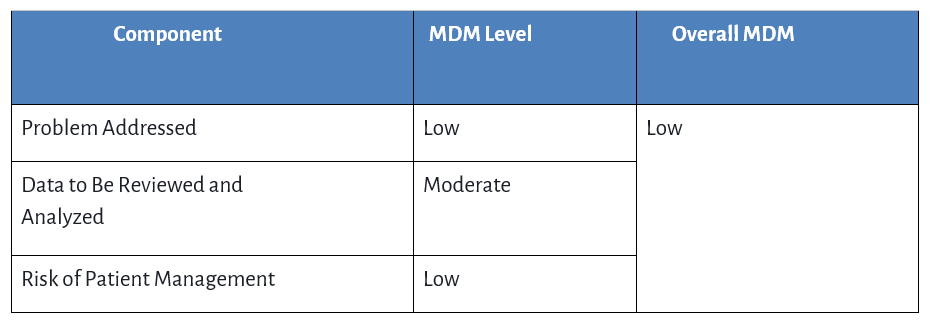
The level of MDM applies separately to each of the MDM components. You are required to have 2 of the 3 components reach a level of MDM to report a given code.
Examples:
Total Time
Total time is the process of adding a time statement to your documentation that includes all the time spent on the date of service (not the time in a 24-hour period) directly caring for one patient. It does not include time spent on activities that can be performed by clinical staff, such as generating a referral or other administrative tasks. It must require the skill and education of a physician or qualified healthcare professional (QHP) such as an NP or PA. If a separately identifiable service is reported, the time spent on that service cannot be included in the total time statement in the documentation (e.g., preventive counseling with CPT codes 99401–99404). The time statement should specify that the time for the visit is independent of the time spent on the separately identifiable services.
Activities
- Preparing to see the patient (eg, review of tests)
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate examination and/or evaluation
- Counseling and educating the patient/family/caregiver
- Ordering medications, tests, or procedures
- Referring and communicating with other health care professionals (when not separately reported)
- Documenting clinical information in the electronic or other health record
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver
- Care coordination (not separately reported)
Documentation Tip: It is not required to document separately how much time was spent on each activity; only a total time statement is required.
Time Statement Examples
Problem-Oriented Visit
Total E/M service time today:_____ minutes
Problem-Oriented Visit with a Procedure
Total E/M service time today:_____ minutes. This time is independent of the time spent performing any procedures.
Preventive Visit with Problem-Oriented Visit
Total E/M service time today:_____ minutes. This time is independent of the time spent providing the preventive service.
Prolonged Service Time
On the Same Date of Service as an E/M Service
Time that is in excess of the time associated with the highest-level code in the set, and code selection was based on a total time statement that exceeded that time by a minimum of 15 minutes. There are 2 codes to report hospital or office based services.
On a Date Separate from an E/M Service
Time spent on a date of service either before or after a related date of service. This is not a face-to-face service and does not require the related E/M to be coded based on time. Consult CPT guidelines for additional information.
MDM or Total Time… How To Choose?
Typically, time will be utilized for visits that were low acuity yet required significant physician time. Some examples might include: visits where when behavioral or mental health conditions (not being addressed) made a physical exam more challenging or required lengthy counseling, the use of interpreter added significant time to visit, or a new parent that had many questions about their child's condition or treatment plan. use MDM If the complexity of the problems, data reviewed, and the risk of treatment drive the service. MDM is used when the clinical complexity best represents the service. It is at the physicians discretion whether or not to report codes based on MDM or total time.
Applying The Guidelines to The Codes
Office or Other Outpatient Services and Outpatient Consultations
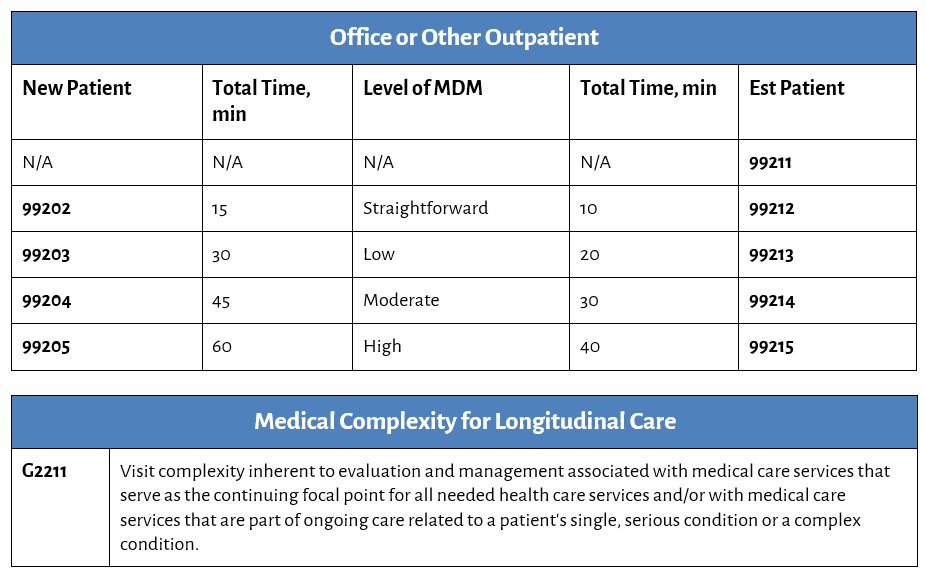
This code is an add on to codes 99202 – 99215. Refer to our factsheet for additional coding and payment resources

Based on payer guidelines, when services are provided via telemedicine, append modifier 93 for audio-only and modifier 95 for audio-visual services or use the telemedicine codes below.
Office or Other Outpatient Telemedicine


Refer to our factsheet on telemedicine codes for additional information.
New vs Established Patients
A new patient is defined as one who has not received any professional services from the same physician/qualified health care professionals within the same group practice, specializing in the same exact specialty and subspecialty, within the past three years.
- A patient who has seen a pediatrician at a multispecialty clinic who has referred them to the psychiatrist who is part of the same practice.
- The last face-to-face professional service was over 3 years ago. Last year the patient came in for a non-counseled flu shot..
An established patient is one who has received professional services from the physician/qualified health care professionals of the exact same specialty and subspecialty who belong to the same group practice, within the past three years.
- You are covering for a pediatrician who is out of town for a few days. You have a coverage arrangement with the pediatrician who is out of town. An established patient of his comes to see you.
- A pediatrician leaves one group practice and joins another pediatric group. Some of her patients follow her to the new practice. One of the patients who followed was established to the pediatrician, presents to the new practice, and sees one of the pediatricians.
Hospital Inpatient, Observation, Discharge, and Consultations

Note: Visits reported with these codes do not have specific telemedicine codes and should have a 93 modifier (audio only) or 95 modifier (audio-visual) appended to the E/M code.
Coding Tip: Well newborn visits provided during the birth admission would be reported with CPT codes 99460-99462. Consult the CPT manual for further information on intensive and critical newborn services.
Emergency Department

Note: ED visits do not use time as a factor in code selection.
Prolonged Service Time

Refer to CPT for conditions that must be met to report these codes.
Coding Tip: Codes for Prolonged service time on a separate date from the E/M apply to the CPT midpoint rule; 99358 is reportable at 31 minutes. And 99359 is reportable at 68 minutes.
AAP Coding Products
The AAP’s Committee on Coding and Nomenclature (COCN) Editorial Advisory Board has developed a wide range of coding products to assist providers and their staff in optimizing charge capture, ensuring clean claims, and facilitating denial management.
Last Updated
09/23/2025
Source
American Academy of Pediatrics