As pediatric clinicians and practices continue to utilize telehealth beyond the pandemic, sustainability and measurement of telehealth programs will continue to become increasingly important. This tip sheet will provide pediatric clinicians and institutions with practical considerations to sustain and measure telehealth beyond the pandemic.
Understanding the Telehealth Program’s Context and Environment
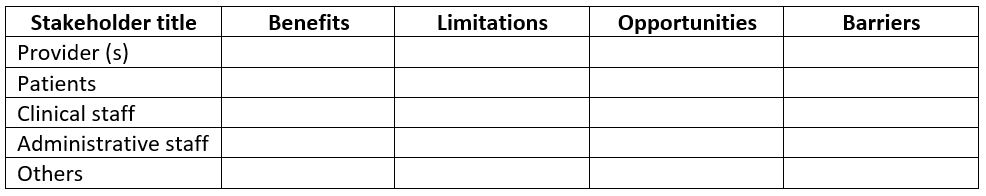
Know the needs and value the perspective of all stakeholders. Arrange to meet with practice team members as well as 1-2 patient and family/caregiver advocates to answer the following questions:
- What is the patient population receiving the care (age, conditions, geographic locations, etc.)?
- Identify the type of visit (preventative, follow-up, other).
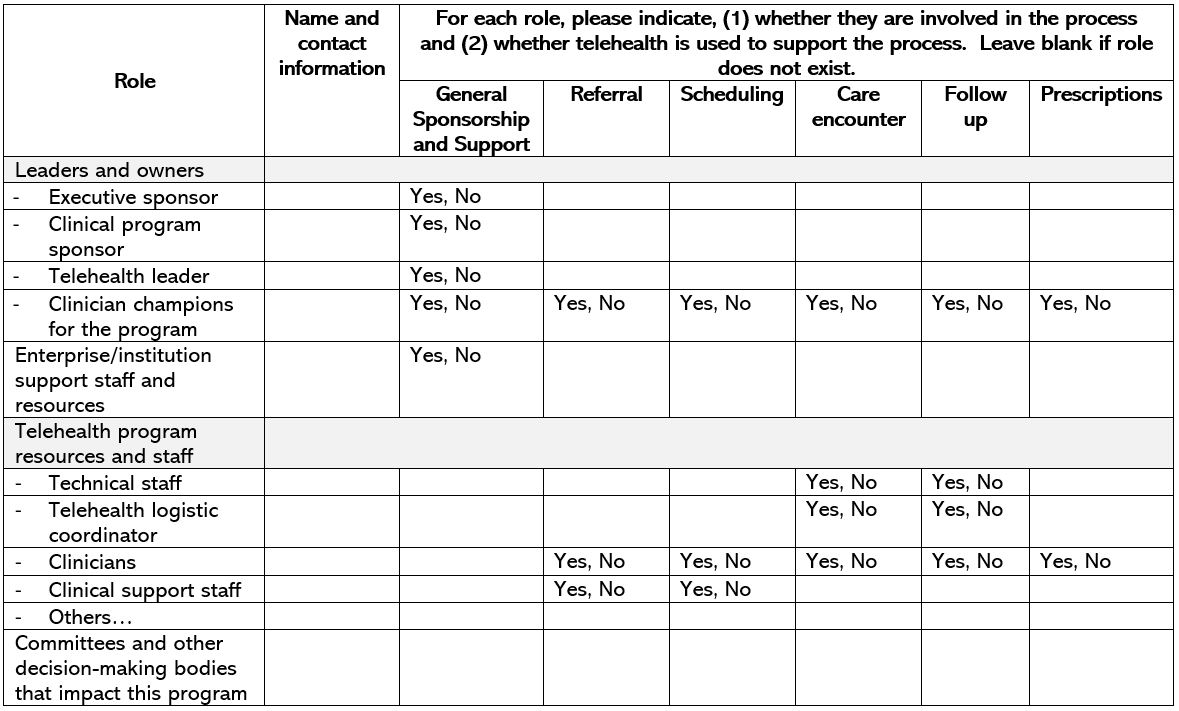
- Who is part of the care team (clinicians, nurses, advanced practitioners, support staff, therapists, etc.) and what are their roles?
- Understand the administrative stakeholders and how their decisions and actions impact the care of these patients (department leaders, hospital, enterprise leaders, policy makers and leaders, etc.).
- Identify the following from each stakeholder’s perspective,
- Has telehealth benefited their patients? If so, how?
- Are there limitations to telehealth? If so, list these limitations.
- Are you willing to continue using telehealth and if so, for what aspect of patient care?
- What would prevent you from using telehealth in your practice?
The goal is to understand which patients are cared for, by whom, and the processes and tools involved in the delivery of that care.
For more details, see the Stakeholder sample table below.
Establish an Effective Sustainment Team
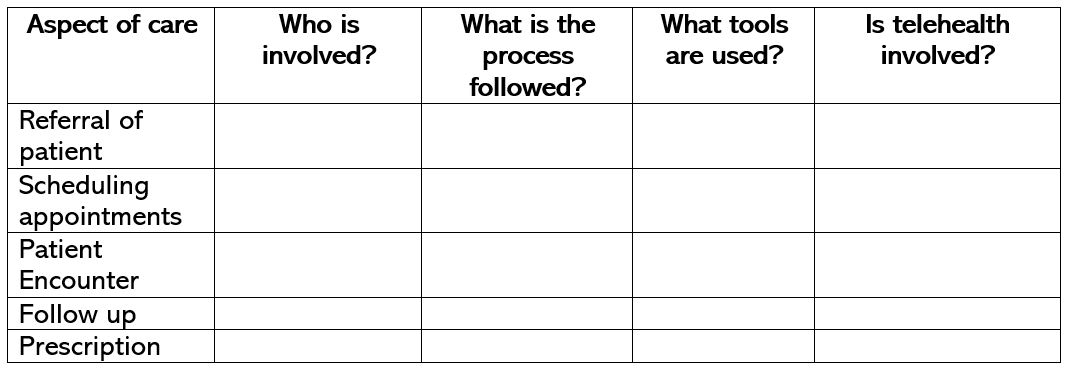
Understand the major aspects of care from the patient/family journey perspective. Whether for inpatient, acute or ambulatory office setting - what are the processes for referrals, signing up as a new patient, making appointments, screening, office intake, provider encounter, follow ups, etc.?
Begin with visualizing the processes related to the aspects of care by using tools such as:
- Workflow diagram
- Swimlane diagram
- Systems map
Are there data on health outcomes of patients being cared for by this team?
Know the role of telehealth. In which aspect of the patient’s care is telehealth involved?
Know your team. Understand each team member’s role in delivering telehealth (refer to your team role sample table).
- Is the team delivering the highest quality of care (safest, patient-centered, effective, efficient, equitable, timely)?
- Are there data to support?
- Where are areas for improvement and can telehealth help or not?
- What tools are used (i.e., electronic medical record system, diagnostic tools, laboratory systems, communication tools, etc.)?
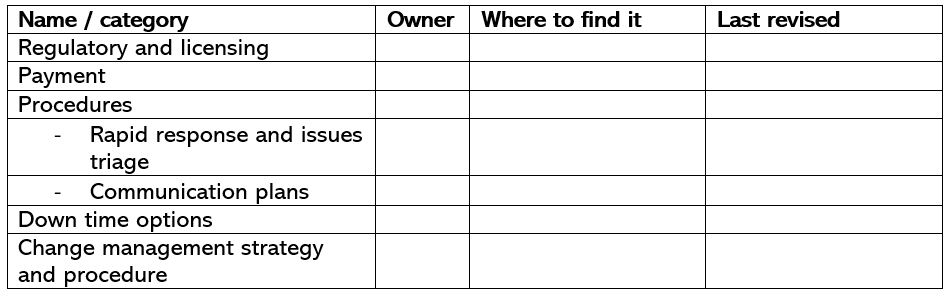
Know the policies and procedures. Identify important policies and procedures.
Measure and Track Progress
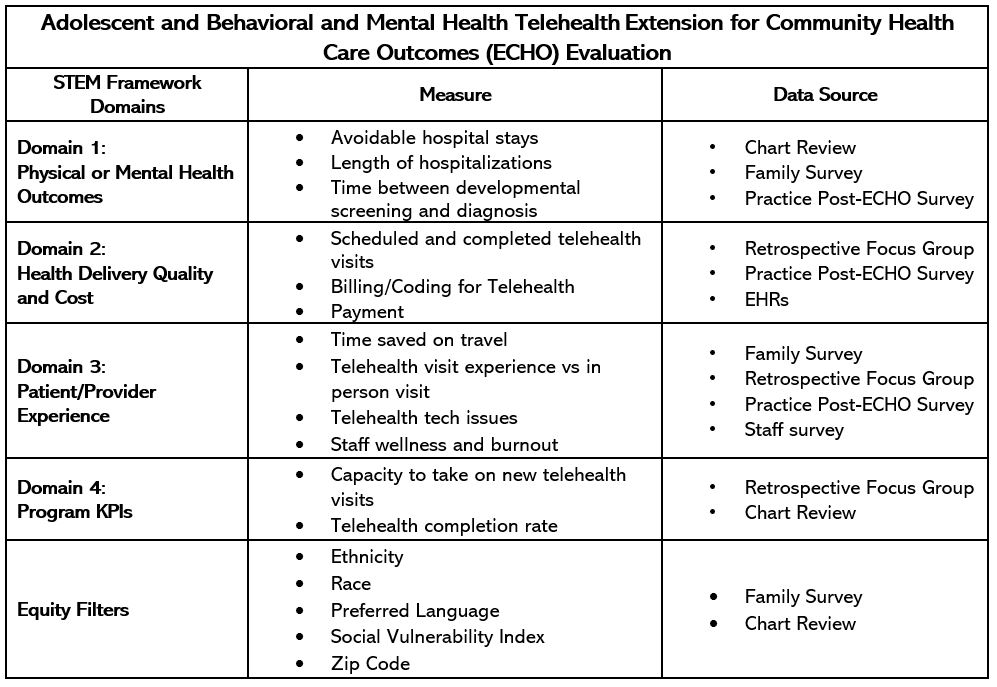
AAP Section on Telehealth Care Supporting Pediatric Research on Outcomes and Utilization of Telehealth (SPROUT) Telehealth Evaluation and Measurement (STEM) Framework is a useful and practical tool for evaluation and sustainability of telehealth using four domains: health outcomes, health delivery value, individual experiences, and key performance indicators.
Implement the STEM Framework. Evaluate the value and effectiveness of your telehealth program and how to use it within your practice to demonstrate value.
- Using the results of steps 1 and 2, identify the STEM profile set of variables to measure:
- Domain 1: Identify 4-7 actionable, collectible health outcome measures of interest for the patient and/or population. Measures should be important to the patient, provider, health system and payers.
- Domain 2: Identify 1 or more measures of health delivery quality and cost (i.e., effectiveness, efficiency, safety, patient centeredness, timeliness or access, cost).
- Domain 3: Identify an aspect of the patient and/or healthcare provider’s experience with the encounter and the technology such as satisfaction, recommendation, usability, feasibility, acceptability (is it possible, doable, and acceptable for ‘live” use).
- Domain 4: Consider what are the program’s key performance indicators (KPIs) that would justify future funding.
- Equity Filters: Define disparity identifier (such as race, ethnicity, social vulnerability indices, etc.). These variables will help you identify sub cohorts of patients on which to measure the STEM variable set.
Data Source: For all domains, determine which measurement tools will be utilized, their data source, and process of collection, including frequency of monitoring and type of reporting.
Note: It is not necessary for practices to measure everything. Identify one measure from each domain that is most important to you. Are there measures you are already tracking for reporting purposes that fits into one of these domains?
- Have ongoing monitoring. Establish a process to monitor and report the above measures (can range from monthly reports to electronic dashboards, etc.).
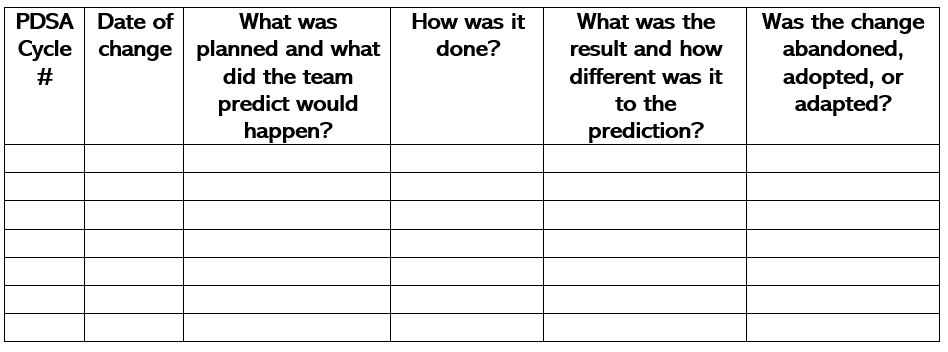
- Use Plan-Do-Study-Act (PDSA) cycles. Use PDSA cycles to implement adjustments to the program in response to data (small to large tests of change based on data driven theory).
Additional Resources
- AAP Section on Telehealth CARE SPROUT Network
- Strategies for Evaluating Telehealth, Chuo et al. Pediatrics, Nov. 2020
- PediaLink Course: Providing Telehealth and Distant Care Services in Pediatrics
- Minimizing Telehealth Technology Barriers in Rural and Underserved Communities
- Ensuring Equitable Access to Telehealth for Diverse and Underserved Communities
This resource is supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) as part of an award totaling $6,000,000 with no percentage financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the US Government.
Last Updated
09/14/2021
Source
American Academy of Pediatrics