Improving the Quality of Developmental Behavioral Pediatrics Office Visits

Dr. Tehrima Rai, MD, MPH, FAAP
June 25, 2025
As a mother of an adorable boy with special needs, I always found myself on edge during office visits with his medical specialists. The visits consumed a lot of energy on my part, primarily because of how my son reacted out of fear to the whole experience. I was distracted and busy managing the tantrums, fear and anxiety that my son experienced during those visits. As a result, I left feeling they had been less productive than I expected and wanted.
While my son was in the middle of a tantrum or anxiety attack, I struggled with staying focused and conveying all my concerns to my doctors, who were giving their best too. Some visits were chaotic with almost minimal to no yield at the end. On my way home, I realized that while I had been prepared before the visit, I forgot to ask my questions or communicate effectively while focused on my son’s uncomfortable experience. I would then have to wait for another 6-8 months for my next visit with hopes it would go better.
The stress of those visits carried through our day. The uncomfortable waiting areas, missed meals, anxiety, transport and all the fear of a ‘hospital’ visit made it worse. I have experienced visiting a general pediatric office and I have not seen any difference in medical office settings designed to treat neurotypical or neurodivergent children.
When I started my fellowship in developmental behavioral pediatrics, I experienced what these visits felt like from the physician’s perspective. The office logistics pose challenges for medical providers and caregivers – but there are ways to improve that.
I also struggled to capture a caregiver’s attention and focus while explaining the complex care and ways to navigate this system to find resources. Parents would leave and forget after-visit summaries, recommendation letters and individualized education plans. I would find them on my desk after we finished the session in the middle of managing a child’s tantrum.
In an ideal world, doctor’s offices should serve as a ‘medical home’ to neurodivergent children and their families.
Improvements can be made to make families feel more at ease in the typically nerve-racking setting of a doctor’s office.
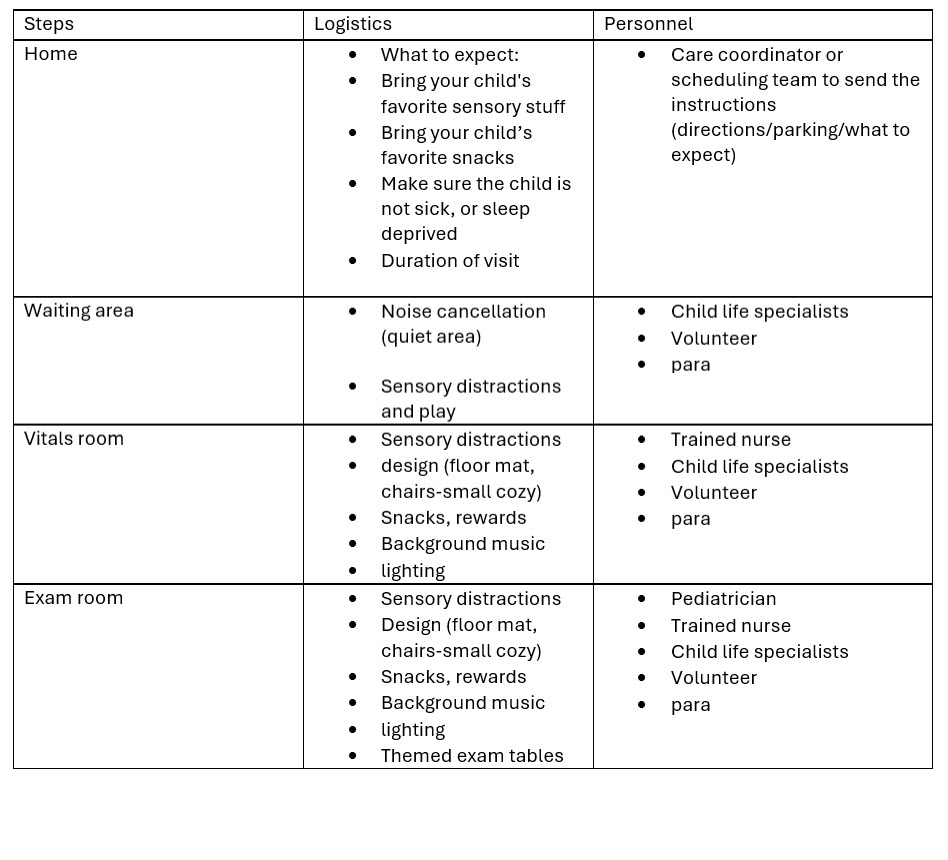
These improvements can also begin at home. As a parent of a special needs child, I prepare for the trip to the doctors well ahead of time to minimize any snags. I plan all logistics, including transportation, transitional objects, sensory toys and snacks.
Pediatric clinics could assist by providing instructions on how to prepare for the visit, like those given before surgery or any minor procedure. Instructions would save parents from a lot of behavioral surprises. To me and many other parents, an evaluation visit feels like a procedure to my neurodivergent child and requires guidance.
At the clinic, busy waiting areas often provoke tantrums because of overcrowded conditions with a lot of noise and distraction. Changes focused on reducing sensory stimulation and play could produce more positive experiences for families.
Once the family gets into a room, the game changes. Fear of a ‘shot’ is at its peak, when a nurse approaches and asks the child to sit. Already overwhelmed with sensory issues, some neurodivergent children will throw a tantrum. Turning vitals room into a sensory room could change the whole experience. Providing rewards or small snacks could help soothe the child and give the provider time to discuss issues with the caregiver.
Just like a vitals room with sensory and transitional modifications, exam rooms and sub-specialty offices could be modified similarly. Additionally, themed exam rooms, such as jungle or garden themed motifs, give a different outlook than a typical hospital doctor’s office and could help to keep both patient and caregiver at ease.
Institutions and leadership would need to propose these changes and qualify for funding to improve quality of care.
Scientific evidence tells us that these calming modifications can improve children's behaviors in any setting. So why not put our knowledge to work in our own clinics?
Let’s work to improve the experience and productivity of the long-waited office visits – starting with developmental behavioral pediatrics clinics.
*The views expressed in this article are those of the author, and not necessarily those of the American Academy of Pediatrics.
About the Author
Dr. Tehrima Rai, MD, MPH, FAAP
Dr. Tehrima Rai, MD, MPH, FAAP, is currently a Fellow in Developmental and Behavioral Pediatrics at the Rose F. Kennedy Children’s Evaluation and Rehabilitation Center at Montefiore. She graduated with an MBBS from Fatima Jinnah Medical University, Lahore, Pakistan and completed residency in General Pediatrics at Bronx Care Health System, affiliated with the Icahn School of Medicine at Mount Sinai, New York. With her master’s in public health from George Washington University, DC and a strong foundation in pediatrics, Dr. Rai is dedicated to advancing equitable, community-centered care for underserved children and families. She is deeply committed to working with children with neurodevelopmental disabilities. her passion lies in providing compassionate, comprehensive care that supports not only the medical but also the developmental and emotional needs of these children and their families.