Research to be presented at the 2021 American Academy of Pediatrics National Conference & Exhibition finds that technology changes during pandemic may have contributed to burnout
ITASCA, IL – A survey of health care providers at a regional pediatric health care network found that the practice changes made in response to the pandemic may contribute to burnout among health care professionals.
The study abstract, “The Impact of COVID-19 and the Rapid Adoption of Telehealth on Provider Burnout in a Pediatric Healthcare Organization,” to be presented during the virtual American Academy of Pediatrics 2021 National Conference & Exhibition, found that those experiencing burnout are more likely to have negative perceptions about telehealth visits.
This may be because the switch to telehealth was done on an emergency basis during the pandemic, and there may not have been enough policies in place to support health care providers, especially for those already experiencing burnout, the authors write. The study also found that institution-level policies to reduce burnout are more likely to be perceived as insufficient by those experiencing burnout.
“Change is hard. The pandemic created the necessity for a massive shift to the adoption of telehealth in health care organizations. There was no time to follow all the rules of change management. Survival and leadership strength fueled change. Recovery must include awareness of the burden of rapid change, plus a crisis, placed on the health care team,” said study author Kenneth Grant, MD, a pediatric gastroenterologist at Children’s Health Orange County.
Previous research on burnout among health care providers has shown that it can have serious negative consequences for health care providers and patients, with clinicians experiencing burnout being more likely to make medical errors, the authors note.
For this study, a brief questionnaire was designed by a multidisciplinary team and sent to all 378 providers at Children’s Health Orange County in June 2020. Eighty-four responded. The survey found that 56% of respondents reported that they were experiencing burnout. The survey also found that 84.5% of respondents believed that their patients seem satisfied with service provided through telehealth. However, more negative perceptions of telehealth increased the odds of reporting burnout by 47%.
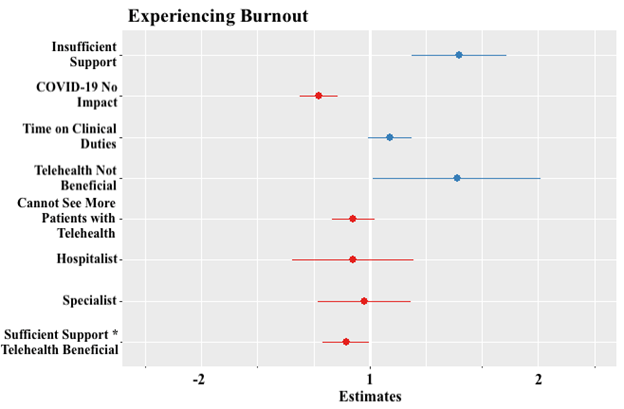
The data show that, when controlling for the other variables in the model, the self-reported experience of burnout is predicted by three perceptions: COVID-19 has exacerbated provider burnout, the benefits of telehealth do not outweigh the challenges, and there is insufficient institutional support to reduce burnout.
Adequate institutional resources for promoting provider well-being, and combating provider burnout, during these difficult times are important, the authors note.
Dr. Tera Reynolds will present the study abstract on Oct. 9, 2021, at 9:55 a.m.
To request an interview, journalists may contact Dr. Kenneth Grant at.
Please note: Only the abstract is being presented at the meeting. In some cases, the researcher may have more data available to share with media or may be preparing a longer article for submission to a journal.
# # #
The American Academy of Pediatrics is an organization of 67,000 primary care pediatricians, pediatric medical subspecialists and pediatric surgical specialists dedicated to the health, safety and well-being of infants, children, adolescents and young adults. For more information, visit www.aap.org.
Program Name:
Abstract Title: The Impact of COVID-19 and the Rapid Adoption of Telehealth on Provider Burnout in a Pediatric Healthcare Organization
Tera Reynolds
Minneapolis, MN, United States
Saturday, October 9, 2021: 9:55 AM –
Clinician burnout is a serious problem in healthcare, which could be exacerbated by the consequences of the ongoing global COVID-19 pandemic, including the abrupt shifts in clinical practice (e.g., rapid increase in telehealth services). It is within this context that we conducted a survey of clinicians at a safety-net pediatric hospital to understand how these factors may have affected providers’ experiences with and perceptions of burnout.
The brief structured questionnaire was designed by a multidisciplinary team and was sent to all 378 providers at CHOC Children’s in June 2020. Questions included demographics, experiences with and perceptions of burnout, and factors that may contribute to or mitigate burnout. After performing descriptive analyses, we used a binomial logistic regression model to test the primary hypotheses of this study: burnout is predicted by both providers’ perceptions of the impact of the COVID-19 pandemic and their perceptions of the consequent transition to telehealth. Provider burnout was measured by the statement, “I am experiencing burnout,” with response options on a Likert scale from Strongly agree to Strongly disagree. This was converted to a binary variable for our analyses. Of note, and as others have done, we chose not to use the 22-item validated measure of burnout to avoid over-burdening clinicians. The study was reviewed and approved by the CHOC Institutional Review Board (#200675).
Eighty-four providers responded (22%), which is typical for surveys of clinicians. The majority of respondents identified as female (57%). Additionally, 70% of participants were between 35 and 54 years old, with about 10% <35 years and 20% >54 years. Almost all respondents (92%) were married or in a domestic partnership. Approximately 46% of respondents were Specialists, 33% General Pediatricians, and 20% Hospitalists. Fifty-six percent of respondents reported that they were experiencing burnout (N=84). Table 1 summarizes key descriptive results, and Figure 1 presents the results of the multivariable logistic regression model predicting self-reported provider burnout. The data show that, when controlling for the other variables in the model, the self-reported experience of burnout is predicted by three perceptions: COVID-19 has exacerbated provider burnout (p<0.001), the benefits of telehealth do not outweigh the challenges (p=0.045), and there is insufficient institutional support to reduce burnout (p<0.001). We also identified a statistically significant interaction, with those perceiving both sufficient institutional support and telehealth to be beneficial being less likely to report experiencing burnout (p=0.045).
Increased institutional support should be provided to clinicians both now, as clinical practice continues to evolve during the COVID-19 pandemic, and more proactively during the inevitable future periods of crisis in an effort to reduce clinician burnout in these difficult times. Future research should assess the effectiveness of different institutional measures on clinician wellbeing.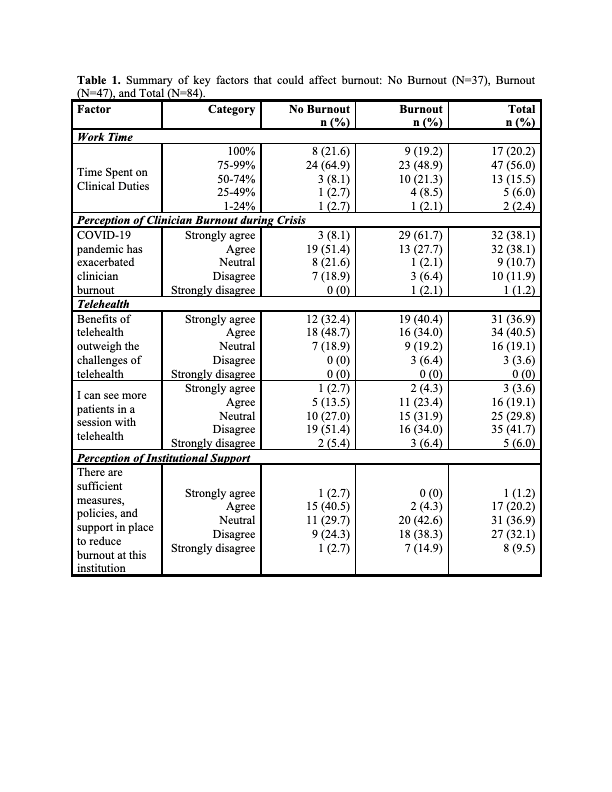
Figure 1. Results from the binomial logistic regression model predicting provider burnout (N=84).