Study showed that staffing changes, pandemic measures may have interfered with breastfeeding in a hospital newborn nursery
ANAHEIM, CA.—The COVID-19 pandemic has had many health impacts on families. While exclusive breastfeeding for the first six months of life is recommended by the American Academy of Pediatrics and the Centers for Disease Control for its benefits to immunity, bonding and health, mothers were less likely to breastfeed during the pandemic, according to research presented during the 2022 AAP National Conference & Exhibition.
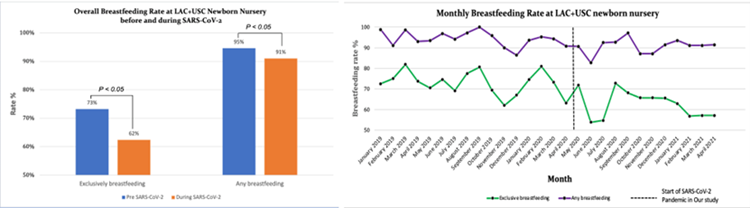
Authors of the abstract, “The Effect of SARS-CoV-2 on the Rates of Breastfeeding in the Newborn Nursery,” found an 11% decrease in the rate of exclusive breastfeeding and a 4% decrease in any breastfeeding during the COVID pandemic in comparison to before.
“There is a false belief that breastfeeding is a natural instinct that’s supposed to happen out of thin air. Breastfeeding is a technique that both the mother and baby need to learn,” said Dr. Amy Yeh, Assistant Professor of Pediatrics, Director of Neonatal-Perinatal Medicine Fellowship Education, Division of Neonatology, Keck School of Medicine of University of Southern California and Attending Neonatologist, LAC+USC Medical Center. “Every mother, baby and dad is unique. It is picking up on the cues of the baby and figuring out what works for both mother and baby. It becomes easier with time. Remember: Mother’s milk is gold.”
This study compared breastfeeding rates between neonates at the LAC+USC Medical Center Newborn Nursery from January 2019 to April 2021. Researchers considered all neonates born prior to April 2020 as pre-COVID babies, comparing breastfeeding rates and trends against infants born during the pandemic. The study found that there were decreases in breastfeeding across all demographic groups studied. Hospital staffing and access to breastfeeding training and other healthcare due to pandemic restrictions were potential causes of the decreased breastfeeding.
“Although a task force was implemented in our newborn nursery immediately after this study to return breastfeeding rates back to normal for our communities, many mothers and newborns missed the opportunity to benefit from the effects of breastfeeding during the pandemic,” Dr. Yeh said.
Study author John Wang, DO, MPH, is scheduled to present a poster on the abstract, which is below, during the Section on Breastfeeding from 12 – 1 p.m. PT Sunday, Oct. 9, 2022. To request an interview with the authors, contact Dr. Wang at [email protected].
In addition, Dr. Wang will be among highlighted abstract authors who will give a brief presentation and be available for interviews during a press conference from 8:30 a.m.- 10 a.m. Saturday, Oct. 8 in the National Conference Press Room, 213 AB. During the meeting, you may reach AAP media relations staff in the Press Room.]
Please note: only the abstract is being presented at the meeting. In some cases, the researcher may have more data available to share with media, or may be preparing a longer article for submission to a journal.
# # #
The American Academy of Pediatrics is an organization of 67,000 primary care pediatricians, pediatric medical subspecialists and pediatric surgical specialists dedicated to the health, safety and well-being of infants, children, adolescents and young adults. For more information, visit www.aap.org. Reporters can access the meeting program and other relevant meeting information through the AAP meeting website at http://www.aapexperience.org/
ABSTRACT
Abstract Title: The Effect of SARS-CoV-2 on the Rates of Breastfeeding in the Newborn Nursery
John Wang
Los Angeles, CA, United States
Exclusive breastfeeding for the first six months of life is recommended by the American Academy of Pediatrics and the Centers for Disease Control for its benefits to infant immunity, maternal-child bonding, and long-term health. While these benefits are well studied, the SARS-CoV-2 pandemic raises questions about the safety of breastfeeding among SARS-CoV-2-positive mothers. In addition, the pandemic’s effects on hospital staffing, patient-provider facetime, and healthcare access may impact breastfeeding rates.
This is a retrospective cohort study comparing breastfeeding rates between neonates at LAC+USC Medical Center Newborn Nursery from January 2019 to April 2021. We defined the pre-SARS-CoV- 2 group as all neonates born prior to April 2020, and the during-SARS-CoV-2 group as those born from April 2020 to April 2021. Maternal data gathered included gravidity and parity, ethnicity, age, mode of delivery, and pregnancy complications. Infant data gathered included gestational age, birth weight, sex, and hyperbilirubinemia requiring intensive phototherapy. Newborns with maternal contraindications to breastfeeding, such as positive toxicology screen, positive HIV status, incarceration, and placement in foster care were excluded. Rates of exclusive breastfeeding and any breastfeeding were calculated for each month within this time period and compared using T-test. P-value less than 0.05 was considered significant.
Of the 964 newborns screened in the pre-SARS-CoV-2 cohort, 913 were included. Of the 800 screened during-SARS-CoV-2 cohort, 763 newborns were included. There were no significant differences in the demographics between the two cohorts (Table 1). We found a 11% decrease in the rate of exclusive breastfeeding (p < 0.05) and a 4% decrease in any breastfeeding (p < 0.05) during the SARS-CoV-2 period (Image 1).
The SARS-CoV-2 pandemic had a negative impact on the rates of both exclusive breastfeeding and any breastfeeding among newborns in the normal nursery from a single center in Los Angeles. These results prompted the creation of a specific task force to counter the detrimental effect of the pandemic on breastfeeding. Prospective studies would be useful in assessing the long-term effects of the SARS-CoV-2 pandemic on breastfeeding rates and associated effects on infant immunity, maternal-child bonding, and long-term health.
Table 1. Maternal and Infant Characteristics
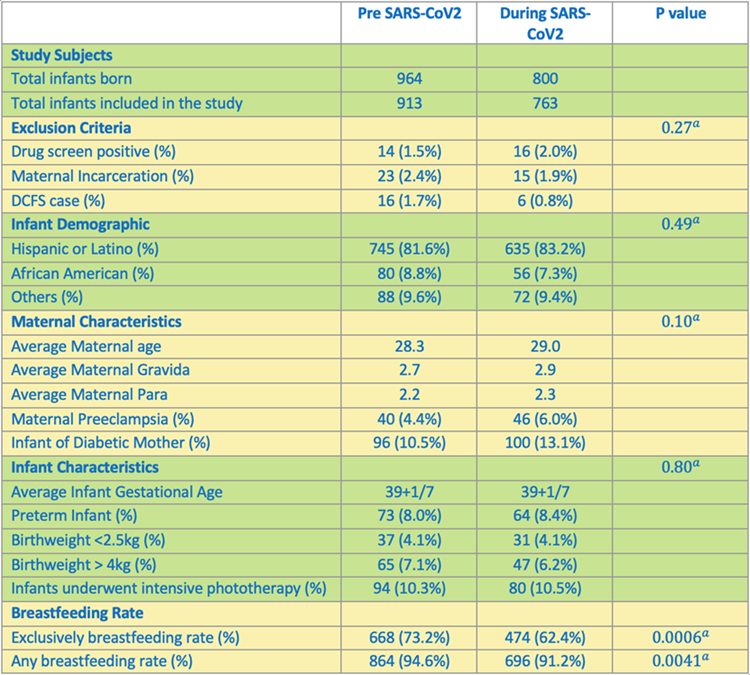
a - Student t-test performed
Image 1. Overall breastfeeding rate at LAC+USC Newborn Nursery before and during SARS-CoV-2 and Monthly breastfeeding rate at LAC+USC Newborn Nursery.