Research presented during the 2022 American Academy of Pediatrics National Conference & Exhibition attributes the uptick in injuries to disruption of family routines and stay-at-home orders during pandemic
ANAHEIM, CA.— Researchers found a significant increase in pediatric injuries sustained while children were engaged in activities where helmets are recommended -- such as bicycling, dirt-biking, skateboarding, snow sports or riding scooters or ATVs – during the COVID-19 pandemic. In many cases, children were not wearing the recommended helmets and sustained serious head injuries, according to the study.
They describe their findings in a study abstract, “Changes in Pediatric Injuries Sustained While Engaged in Activities Where Helmet Usage Is Recommended During the COVID-19 Pandemic,” to be presented at the 2022 American Academy of Pediatrics National Conference & Exhibition.
The research analyzes data from two large pediatric trauma centers, finding a trend towards decreased helmet use, increased associated head injuries, and increased neurosurgical consultations.
“The COVID-19 pandemic led to a significant disruption in the daily lives and routines of families in our patient population,” said Brent Troy MD, MPH, FAAP. “Our data highlights that this likely contributed to an increase in pediatric injuries for children engaged in activities with recommended helmet usage, such as bicycling and scootering.”
The authors found a 37% increase in pediatric injuries between 2018 to 2020 resulting from activities where helmet use is encouraged. In 2020, there were 420 pediatric injuries as compared with 263 injuries reported in 2018.
Within the local hospital-system’s pediatric patient population, researchers saw a rate of 1.85 injuries per 10,000 pediatric patients in 2018, as compared to 3.43 injuries per 10,000 pediatric patients during the COVID-19 pandemic. They also noted an increase of head injuries (56 in 2018 to 140 in 2020) and severe head injuries requiring neurosurgical consultation (17 in 2018 to 87 in 2020).
Overall, the increase in injuries seemed most problematic for those that were publicly insured (104 injuries in 2018 to 252 injuries in 2020), according to the abstract.
With children no longer being in child care or school due to COVID-19 related closures, family dynamics were likely altered, resulting in children spending more time at home, where they were able to engage in activities like bicycling, potentially with less supervision than typical. They suggest that more research is needed, with a focus on the increase in Medicaid patient population.
Dr. Troy is scheduled to present an abstract of the study, available below, during an oral presentation between 3:45 p.m.-5 p.m. PT Sunday, Oct. 9, during the Session on Injury, Violence, and Poison Prevention at Anaheim Convention Center Room 262. To request an interview with the author, journalists may contact him at [email protected] or call Amy Marriott at Children's Healthcare of Atlanta, 404-785-7936.
In addition, Dr. Troy will be among highlighted abstract authors who will give brief presentations and be available for interviews during a press conference from 8:30 a.m.-10 a.m. Sunday, Oct. 9, in the National Conference Press Room, 213 AB. During the meeting, you may reach AAP media relations staff in the Press Room.
Please note: only the abstract is being presented at the meeting. In some cases, the researcher may have more data available to share with media, or may be preparing a longer article for submission to a journal.
# # #
The American Academy of Pediatrics is an organization of 67,000 primary care pediatricians, pediatric medical subspecialists and pediatric surgical specialists dedicated to the health, safety and well-being of infants, children, adolescents and young adults. For more information, visit www.aap.org. Reporters can access the meeting program and other relevant meeting information through the AAP meeting website at http://www.aapexperience.org/
Program Name: 2022 AAP National Conference & Exhibition
Abstract Title: Changes in Pediatric Injuries Sustained While Engaged in Activities Where Helmet Usage Is Recommended During the COVID-19 Pandemic
Brent Troy
Atlanta, GA, United States
Unintentional injuries, including traumatic-brain-injuries (TBI), are the leading cause of pediatric morbidity and mortality in the United States. Helmet use in activities, such as bicycling, scootering, snow sports, skating, horseback riding, and all-terrain-vehicles (ATVs) riding, can reduce TBI incidence and severity. Epidemiology surrounding TBI and helmet use is ever-evolving, and changes may have been further accelerated by the COVID-19 pandemic that altered family lifestyles including access to resources, finances, family activities, and supervision of children; however, this has not been studied in-depth.
Utilizing the trauma registries from 2 large, metropolitan pediatric hospitals within a single healthcare system during 2018-2020, we retrospectively compared patients presenting with injuries sustained during activities where helmet use is recommended (AWHUR). AWHUR included mechanisms such as bicycling, ATVs, horseback riding, dirt-biking, skateboarding, skating, and snow sports. Inclusion criteria were patients aged 0 to 18 years old who met national trauma registry criteria and were injured while participating in AWHUR.
Abstracted data included demographics, insurance status, activity type, helmet use, presence of head injury, and extent of head injury, including neurosurgical consultation. Data was analyzed for a 9.5-month period each year to compare the same period pre-COVID and in concordance with the statewide declared closure of schools and recreational facilities during the pandemic.
A total of 1093 patients presented with injuries from AWHUR over 3 years (Table 1). AWHUR injuries increased annually from 263 patients in 2018 to 492 in 2020 (Table 1, Figure 2 Graph A&B). The most frequently implicated mechanisms included bicycles (35.9%), ATVs (20.3%), skateboards (11.6%), scooters (8.3%), and dirt-bikes (7.4%) (Table 1, Figure 2 Graph A&B). There was an increase in unhelmeted patients from 111 (58.7%) in 2018 to 258 (64.8%) in 2020 (Table 1, Figure 2 Graph B). A significant increase in neurosurgical consultation was found from 17 (6.5%) patients in 2018 to 87 (17.7%) patients in 2020 (p=0.021) (Table 1). The proportion of patients who presented with head injuries and without wearing a helmet increased pre-pandemic to during the pandemic (Table 1). Additionally, there was a notable increase in the percentage of patients with Medicaid presenting from AWHUR injuries during the pandemic (p< 0.001) (Table 1).
This study found an increase in patients presenting with injuries sustained whilst engaged in AWHUR in relation to the COVID pandemic. Concerningly, there was a trend towards decreased helmet utilization, increased associated head injuries, and increased neurosurgical consultations. There remains a critical need to improve helmet usage in AWHUR through helmet campaigns, due to the increase in the number of AWHUR injuries and decreased helmet usage during the pandemic. Further analysis is needed into the communities impacted by AWHUR related head injuries, from the pandemic, with focus on the increase in Medicaid patients.
AWHUR Patient Demographics, Injury Mechanisms, and Head Injury Data Table
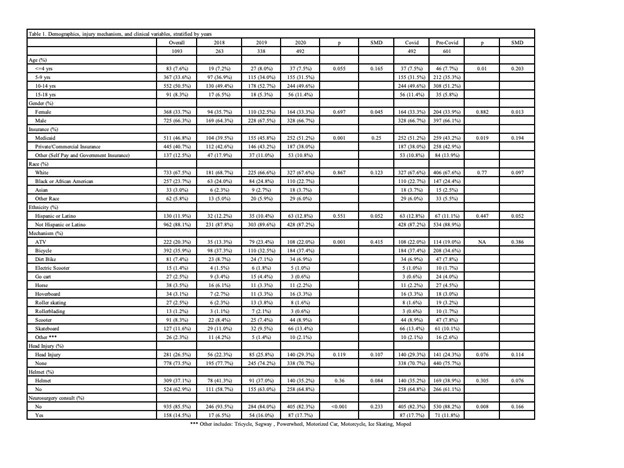
AWHUR table of patient information with regards to demographics, injury mechanisms, and head injury related data from years 2018 to 2020 and in relation to the COVID pandemic.
Top AWHUR Injury Mechanisms from 2018 to 2020
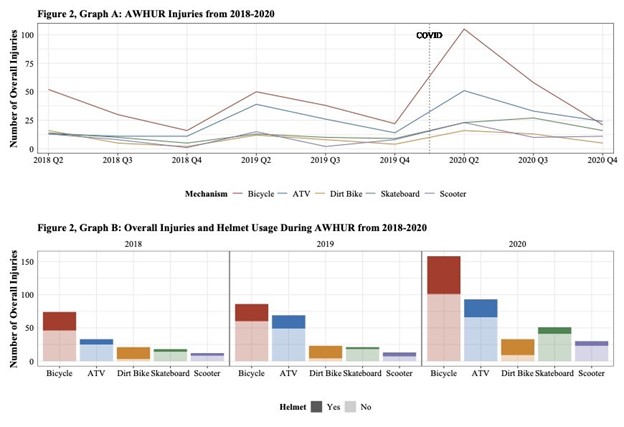
Graph A demonstrates the trend in top AWHUR mechanisms from 2018 to 2020 with a line indicating when the COVID-19 pandemic began along the timeline. Graph B demonstrates the number of patients who presented via the most frequent AWHUR mechanisms from 2018 to 2020. Graph B also includes the breakdown of patients wearing a helmet versus not wearing a helmet for the top AWHUR mechanisms.
##