It is important to know how to code and be paid for the administration and counseling.
Refer here for further details on coding for COVID-related encounters.
COVID Vaccine Coding
Coding for Services Related to COVID-19 Vaccines and Immunization Administration
Vaccine Product and Administration
Pediatricians who administer COVID-19 vaccines in their practice can get paid for vaccine administration by following the steps outlined below.
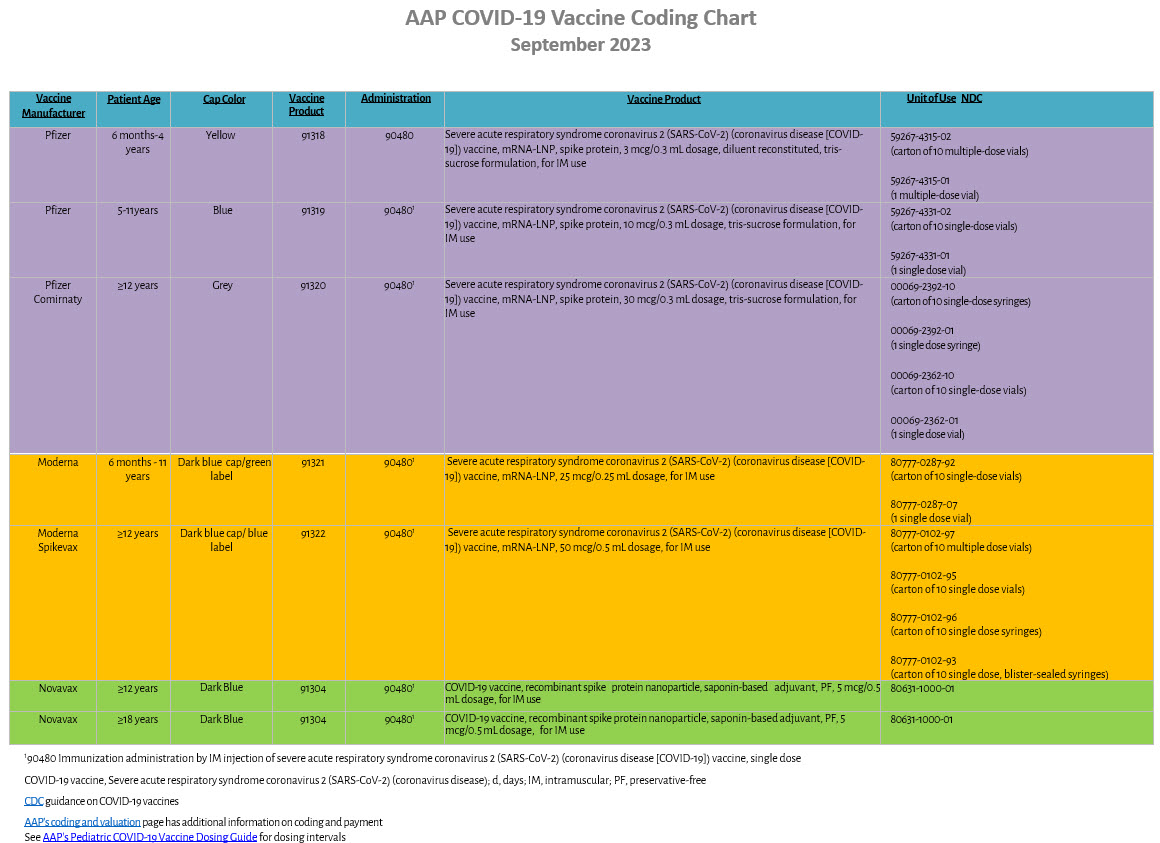
The CPT Editorial Panel has developed several new SARS-CoV-2 vaccines product codes and a single immunization administration codes. The CPT codes clinically distinguish each coronavirus vaccine product and the specific dose for better tracking, reporting, and analysis. The CPT codes for the administration includes:
- practice expense costs of storage and ordering
- counseling provided to patients or caregivers on the date the vaccine is administered
- administering the vaccine
- updating the electronic health record and the vaccine registry
Note you will not report the immunization administration codes (90460-90461, 90471-90474) when administering a COVID-19 vaccine.
Vaccine Counseling Coding
Vaccine Counseling Without Vaccine Administration
There may be occasions when a patient or parent presents to their medical home for vaccine counseling, particularly for the COVID-19 vaccine. Increasing vaccine hesitancy surrounding this vaccine may be greater, and some older adolescents may seek out information on their own. For patients and caregivers who opt for in-person (i.e., in-office or telehealth) individual counseling, there are coding options. Note, if you provide vaccine counseling on the day you also administer the vaccine to the patient, you may not report counseling separately since code 90480 is valued to include counseling.
If separately identifiable services related to an illness are provided you would report an E/M from code range 99202 – 99215 based on MDM, add a 25 modifier, and report the counseling based on documented time relating to counseling with code range 99401 – 99404.
OR
If separately identifiable services related to an illness are provided, you would report an E/M from code range 99202 – 99215 based on time, add a 25 modifier, and report documented time for the counseling by including it in your time for the illness-related visit.
Please note that if you combine the time for the E/M and counseling, this could increase the level of service and increase the patient's cost share for what should be a preventive service, which is covered at no cost share for the patient.
ICD-10-CM codes
Z71.85 Encounter for immunization safety counseling
Plus a code from the following:
Z28.01 Immunization not carried out because of acute illness of patient
Z28.02 Immunization not carried out because of chronic illness or condition of patient
Z28.03 Immunization not carried out because of immune compromised state of patient
Z28.04 Immunization not carried out because of patient allergy to vaccine or component
Z28.09 Immunization not carried out because of other contraindication
Z28.20 Immunization not carried out because of patient decision for unspecified reason
Z28.21 Immunization not carried out because of patient refusal
Z28.29 Immunization not carried out because of patient decision for other reason
Z28.82 Immunization not carried out because of caregiver refusal
Z28.83 Immunization not carried out due to unavailability of vaccine
Vaccine Counseling with Vaccine Administration
If the entirety of the visit consists of counseling and administration of the vaccine, report one of the appropriate product codes 91304 or 91318 – 91322 and the administration code 90480. There is no additional code to report for counseling, as 90480 has been valued to include counseling.
If additional E/M services were provided, code selection is based on documentation:
Problem related E/M visit for a separately identifiable illness would report the appropriate codes from range 99202 – 99215, add a 25 modifier, an appropriate product code, and 90480 for administration and counseling for the vaccine.
Periodic preventive E/M codes from range 99381 – 99384(new patient) or 99391 – 99394(established patient), add a 25 modifier, an appropriate product code, and 90480 for administration and counseling for the vaccine.
Coding Tips:
- Report only one vaccine administration code per COVID-19 injection
- Your ICD-10-CM code for COVID-19 vaccine administration is Z23 - Encounter for immunization.
CPT Coding Vignettes for COVID Vaccine Administration Encounters
Vignette #1
A 6-year-old patient presents 2 days after their routine wellness visit for administration of the COVID-19 vaccine.. The patient receives their first Pfizer 2023/2024 COVID-19 vaccine of 10 mcg/0.3 mL dosage.
Report CPT codes:
91319 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease [COVID-19]) vaccine, mRNA-LNP, spike protein, 10 mcg/0.3 mL dosage, tris-sucrose formulation, for IM use
90480 Immunization administration by IM injection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease [COVID-19]) vaccine, single dose
Vignette #2
A 7-year-old patient presents for the administration of a COVID-19 vaccine. The physician counsels the parent on the risks and benefits of receiving COVID-19 vaccine. All of the parents’ questions are documented and answered. The parent declines the COVID-19 vaccine due to perceived risks involved.
Report CPT codes:
99401-99404 Preventive Medicine Counseling: based on time spent counseling
Vignette #3
A 13-year-old established patient presents for a well-child visit. A preventive service is provided, including documentation of the child’s BMI and counseling for healthy diet and exercise. The physician also counsels for immunization against COVID-19. The patient previously had one dose of a Moderna bivalent COVID-19 vaccine. The Moderna 2023/2024 vaccine of 50 mcg/0.5 mL dosage is administered at the encounter.
Report CPT codes:
99394 Periodic comprehensive preventive medicine reevaluation and management of an individual, established patient; adolescent (age 12 through 17 years)
91322 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease [COVID-19]) vaccine, mRNA-LNP, 50 mcg/0.5 mL dosage, for IM use
90480 Immunization administration by IM injection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease [COVID-19]) vaccine, single dose
Note:
Include a 25 modifier on 99394.
Vignette #4
A 16-year-old established patient presents for management of ADHD. Before the end of the visit the physician counsels the parent on the risks and benefits of being vaccinated for COVID-19. The parent agrees with vaccinating their child and the patient receives a 5 mcg/0.5 mL dose of the 2023/2024 Novavax vaccine.
Report CPT codes:
Appropriate E/M from codes 99212 – 99215
91304 COVID-19 vaccine, recombinant spike protein nanoparticle, saponin-based adjuvant, PF, 5 mcg/0.5 mL dosage, for IM use
90480 Immunization administration by IM injection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease [COVID-19]) vaccine, single dose
Note:
Include a 25 modifier on selected E/M code.
What Will I be Paid?
The CMS initially published Medicare payment amounts for administration of COVID-19 vaccines of $16.94 for administration of the first dose, and $28.39 for the second dose (and $28.39 for the administration of single-dose COVID-19 vaccines). On March 15, 2021, it was announced that Medicare is updating these payment amounts to $40 for each COVID-19 vaccine administration (ie, $40 for each injection, a total of $80 for those requiring two doses). This data is current as of 7/25/23. Beginning January 1, 2024, Medicare payment for the administration of COVID-19 vaccine will be set at a level that aligns with the Medicare payment rate for other Part B preventative services (approximately $30).
Related, the American Rescue Plan Act (ARPA), signed into law on March 11, 2021, raises the federal medical assistance percentage (FMAP) for all COVID-19 vaccine administered to Medicaid and CHIP enrollees to 100% beginning April 1, 2021 through September 30, 2024, thus, making COVID-19 vaccine administration free to states for these populations. All Medicaid and CHIP programs should update their fee schedules to pay for the administration of COVID-19 vaccine at levels at least equal to Medicare payment. Advocacy through your AAP chapter may be needed if this is not occurring.
In private plans, pediatricians should work with payers with whom they contract to ensure they are paid appropriately for the administration of COVID-19 vaccine.
Last Updated
09/19/2023
Source
American Academy of Pediatrics