Gerber JS, Hersh AL, Grundmeier R, Szymczak JE, Mayne S, Frager N, Wright M, Steffes J, Frantz JM, Shone L, Fiks A
Accepted for 2020 Pediatric Academic Societies Annual Meeting
Background: At least 30% of antibiotic prescriptions for pediatric acute respiratory tract infections (ARTIs) are unnecessary. Many outpatient stewardship interventions have focused on reducing prescribing for conditions coded as viral infections. However, diagnosis rates for bacterial ARTIs (e.g. acute otitis media, sinusitis) remain widely variable, reflecting the approach's limitations in addressing overdiagnosis of bacterial infections.
Objective: Explore variability in diagnosis and antibiotic prescribing for ARTIs across pediatric primary care practices. Results will be used to inform a benchmark for total antibiotic prescribing rates for all ARTIs to inform outpatient antibiotic stewardship efforts.
Methods: We examined diagnoses and antibiotic prescribing for common ARTIs in children 6 months-12 years who presented for acute care to pediatric primary care practices from Jan 1, 2014-Dec 31, 2016. EHR data from the AAP Comparative Effective Research through Collaborative Electronic Reporting (CER2) database were utilized. CER2 includes a diverse population from urban, suburban, and rural settings across 27 US states. We included antibiotic prescribing that occurred during an in-person encounter for an ARTI, defined by an ICD9/10 code for viral (acute nasopharyngitis, unspecified lower respiratory infections, unspecified upper respiratory infections, bronchiolitis, bronchitis, croup, influenza, laryngitis, tracheitis), and potentially bacterial (pharyngitis, acute otitis media (AOM), sinusitis, and pneumonia) infections. Antibiotic prescribing and ARTI diagnosis rates were standardized by patient age and sex using fixed-effect logistic regression models and marginal standardization.
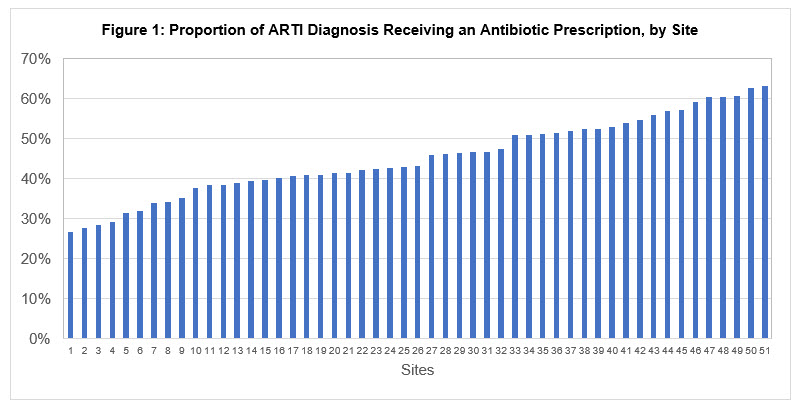
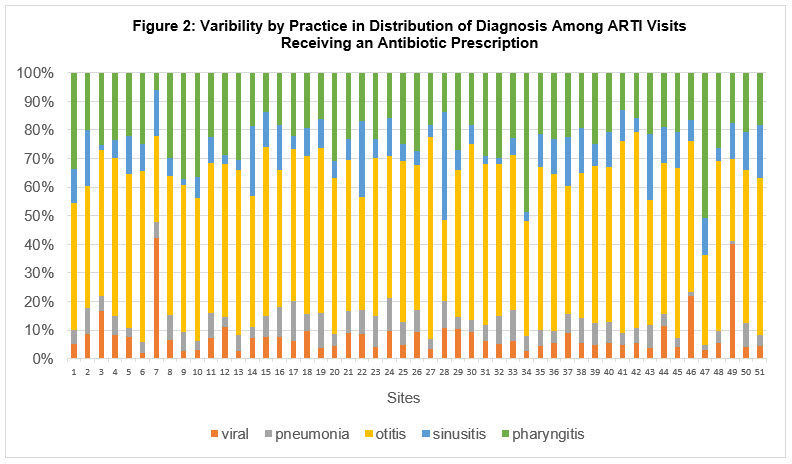
Results: 51 sites and 2,583,053 patient encounters were included. Viral infections accounted for 36.6% (IQR 33.2-47.4%) of ARTI diagnoses across practices, followed by AOM (28.9%; 24.8-33.7%), pharyngitis (22.1%; 17.6-28.9%), sinusitis (5.6%; 3.1-5.9%), and pneumonia (3.1; 2.7-3.6%). By site, the proportion of ARTIs for which antibiotics were prescribed ranged from 26.8% to 63.1% (Fig 1). Rates of specific ARTI diagnosis varied widely by site (Fig 2).
Conclusions: Rates of antibiotic prescribing for ARTIs and the distribution of diagnoses for ARTIs varied widely by practice. The data illustrate the importance of tracking both diagnosis and prescribing patterns for effective antibiotic stewardship and provide ranges for each to inform future benchmarks.
Last Updated
10/08/2021
Source
American Academy of Pediatrics