Wittman S, Kelly MK, Ramachandran J, Davis K, Harris D, Steffes J, Biel F, Macario E, Hatch B, Szymczak, Yabes JG, Grundmeier R, Fiks AG, Ray KN
Presented at the 2025 Pediatric Academic Societies Annual Meeting
Background: Since the telemedicine policy changes that occurred with the COVID-19 pandemic, many primary care practices have integrated telemedicine (TM) along with in-person (IP) visits. Previous work raised concerns about the quality of antibiotic management for pediatric acute respiratory tract infections (ARTIs) in direct-to-consumer telemedicine visits, which occur with virtual-only vendors. However, emerging data from single health systems suggest antibiotic prescribing may be more judicious when TM is integrated within primary care practices.
Objective: To compare antibiotic management during TM and IP visits for ARTIs among children within heterogenous primary care practices.
Methods: We performed retrospective, cross-sectional analyses of 2023 electronic health record data from 843 U.S. pediatric and family medicine primary care sites with diverse geography and patient populations. We identified TM and IP visits by children <18 years for bacterial and viral ARTIs and constructed episodes of care, defined as an index visit (visit with no ARTI visit in prior 21 days) and any follow-up visits (visits in subsequent 14 days). We compared antibiotic receipt, diagnoses, guideline concordant antibiotic management, and follow-up care for episodes with TM vs IP index visits. We used logistic regression with patient-level random intercepts to test the significance of differences.
Results: We analyzed 540,607 ARTI episodes, after excluding episodes where the index visit was a well visit (7%) or had co-diagnoses that could warrant antibiotics (3%; Figure 1). Episodes were 48.3% for children insured by Medicaid, 10.8% with Spanish-speaking families, and 2.3% via TM (Table 1).
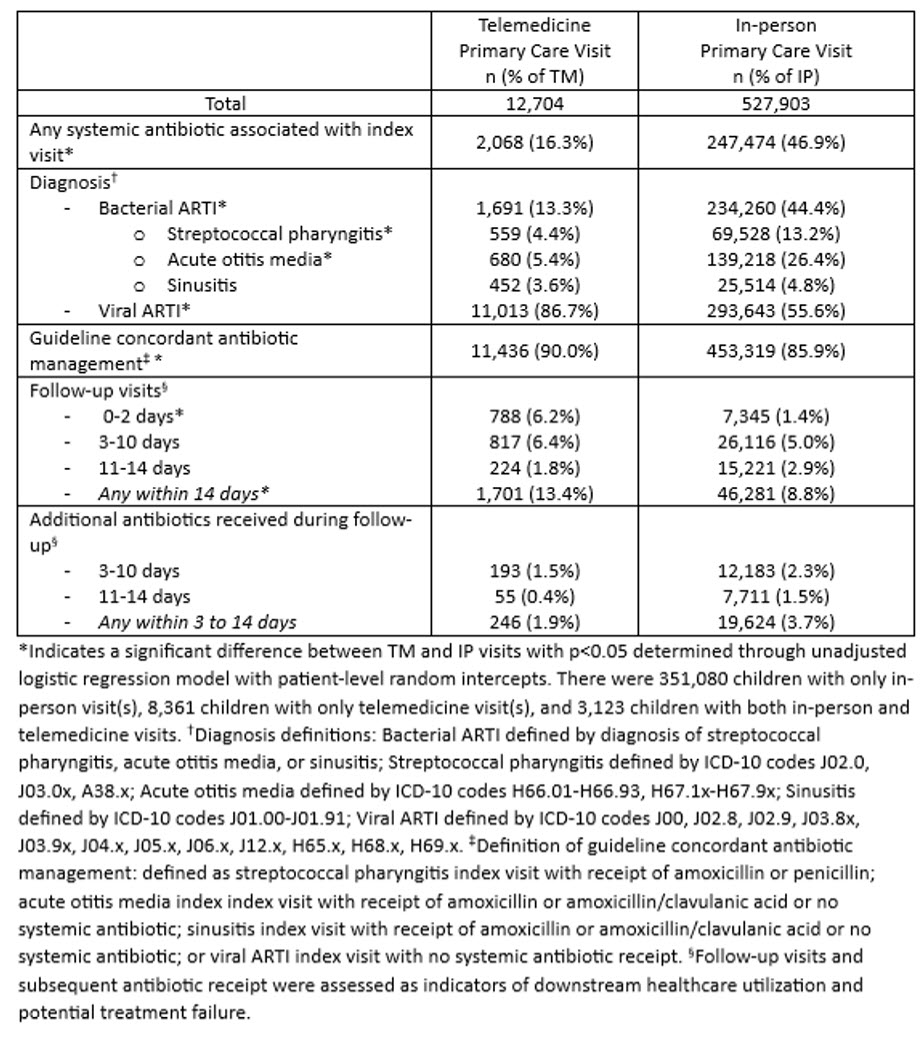
Compared to IP index visits, TM index visits were less likely to receive an antibiotic prescription (16.3% TM vs 46.9% IP, p<.001) and less likely to receive bacterial diagnoses (13.3% TM vs 44.4% IP, p<.001). Of bacterial diagnoses, acute otitis media was diagnosed most often (5.4% TM; 26.4% IP), then streptococcal pharyngitis (4.4% TM; 13.2% IP) and sinusitis (3.6% TM; 4.8% IP). TM index visits had slightly higher rates of guideline concordant antibiotic management (90.0%) than IP index visits (85.9%, p<.001). In the 14 days after the index visit, TM index visits had higher rates of follow-up visits, but did not have significantly more subsequent antibiotic prescriptions (1.9% TM vs 3.7% IP, p=.15).
Conclusion: Despite concerns about antibiotic prescribing for children via TM with direct-to-consumer virtual-only vendors, we found evidence of judicious antibiotic prescribing for children during TM integrated within primary care practices.
Figure 1. Flow Diagram of Included Episodes
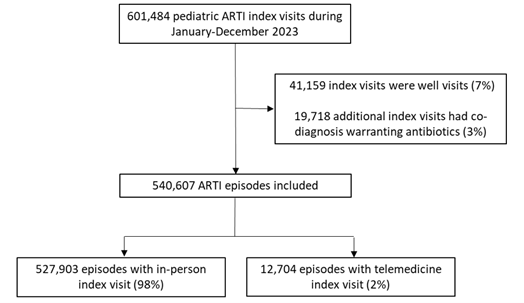
Table 1. Index Acute Respiratory Tract Infection Visit Characteristics
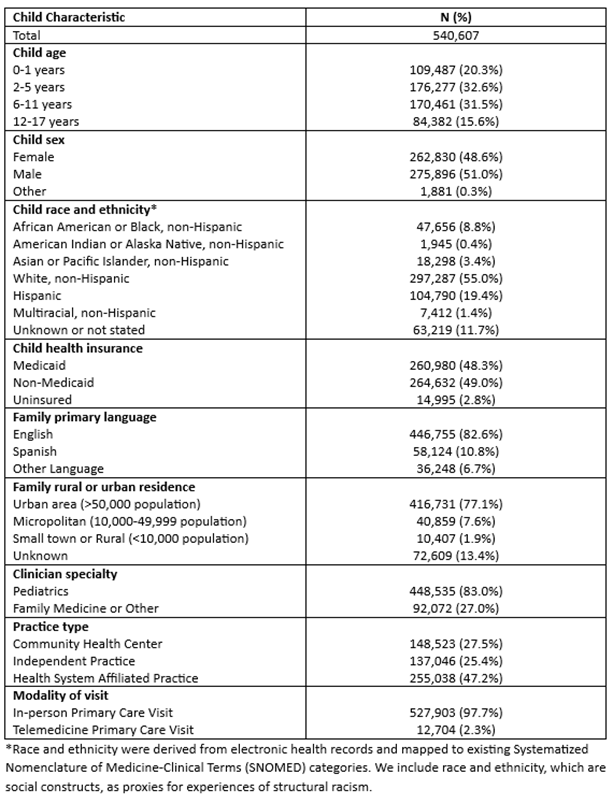
Table 2. Acute Respiratory Tract Infection Episode Outcomes, by Index Visit Modality
Last Updated
05/15/2025
Source
American Academy of Pediatrics