Emerson Delacroix, Margaret Wright, Kendrin R. Sonneville, Melissa S. Stockwell, Heide Woo, Laura P. Shone, Jenny Steffes, Donna Harris, Ken Resnicow
Presented at the 2019 Pediatric Academic Societies Annual Meeting.
Background: Primary care remains an important, underutilized venue for treatment of pediatric obesity. Our prior trials showed a significant impact of primary care provider (PCP) and Registered Dietitian (RD)-delivered motivational interviewing (MI) on reduction of child body mass index (BMI).
Objective: To understand child nutrition and activity behaviors reported by parents enrolled in a BMI reduction intervention.
Methods: Parents of 3-12 year old children with a BMI >85th percentile were recruited into a 2-year NIH-funded intervention (BMi2+) in which PCPs and RDs provide up to 10 MI counseling sessions focused on nutrition, physical activity, and/or screen time. Practices (n=18) were from the national AAP PROS practice-based research network. In a baseline survey, parents from the 9 intervention group practices reported demographics and graded their child’s nutrition and activity behaviors as A (great) - F (poor), and rated concerns about their child’s weight, as well as confidence in achieving their related goals, on a scale of 0 (not at all) - 10 (very). Differences by income and race/ethnicity were compared using chi square and ANOVA.
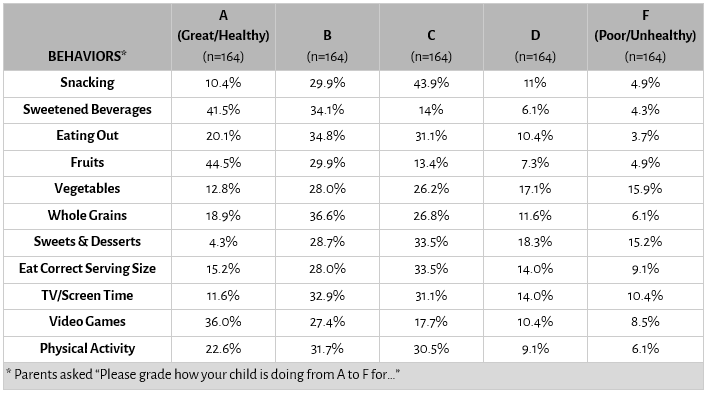
Results: We analyzed data from the first 164 parents completing the survey. In this demographically diverse sample, parents most often gave their children an A on fruit and sugar sweetened beverages (SSB) consumption and F for sweets and vegetables (Tables 1 and 2). Parents with higher reported income were more likely to give their child an A for whole grains and SSB (p<0.05); parents of White, non-Latino vs. Latino children were more likely to give their child an A (61% vs. 25%; p<0.05) on SSB. Parents were fairly confident their child would achieve a healthy weight (7.2 ± 2.1) and change their eating (7.3 ± 2.2), activity (7.4 ± 2.0), and TV time (6.9 ± 2.5). There were no differences in parent confidence by race or income. Parent level of concern about their child’s weight (4.8 ± 3.4) was higher than they perceived their child’s level of concern to be (2.8 ± 3.2). Parents with higher income were less concerned about their child’s weight (r=-0.23, p<.05); there were no differences by child race.
Conclusion: In this diverse sample of parents enrolled in a weight-related study, parents highlighted several child nutrition and activity challenges, and were more concerned than they perceived their child to be. However, overall parents had confidence they could make changes to positively impact their child’s behavior.
Table 1. Baseline characteristics of parent participants and their children in the BMI2+ study intervention group (n= 164)
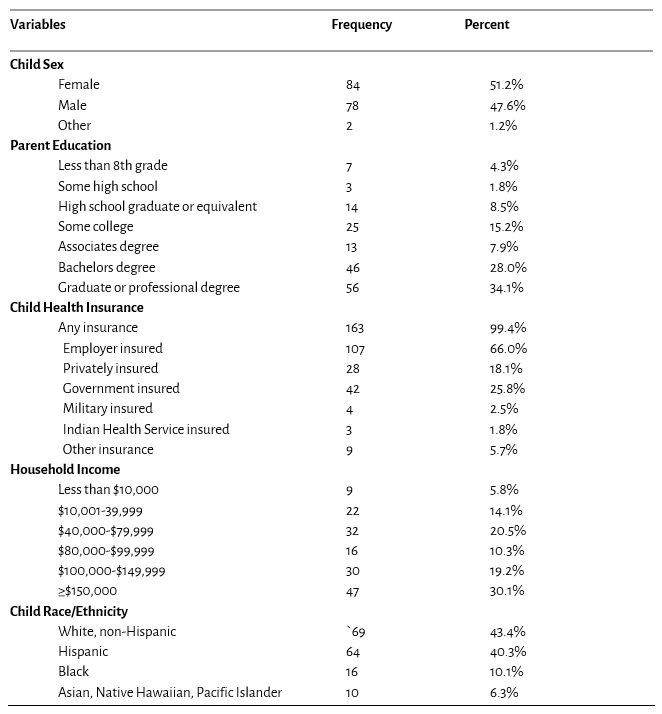
Table 2. Parent-assigned grades at study baseline for child nutrition and activity behaviors in the BMI2+ study intervention group
Last Updated
10/08/2021
Source
American Academy of Pediatrics