Tang S, Cull WL, Larson K, Gottschlich EA, Olson L
Accepted for 2020 Pediatric Academic Societies Annual Meeting
Background: ADHD, anxiety and depression are common pediatric mental disorders linked to an increased risk of suicide. Diagnosing and treating these conditions is vital for pediatric health and suicide prevention.
Objectives: Examine trends in the diagnoses of 3 mental health disorders in the pediatric population and investigate whether trends remain when controlling for patient demographic factors, as well as increases in insurance coverage.
Design/Methods: We used the Medical Expenditure Panel Survey to create a nationally representative sample of US persons ages 6-21 (n=167,671) matched with diagnoses from all care settings. We described changes in ADHD, anxiety and depression diagnosis rates over 3 survey-year cohorts (1997-2003, 2004-10, 2011-17). We used bivariate comparisons and multivariable logistic regressions to examine diagnosis trends while controlling for patient/family income, health insurance coverage, age, sex, race/ethnicity and geographic region.
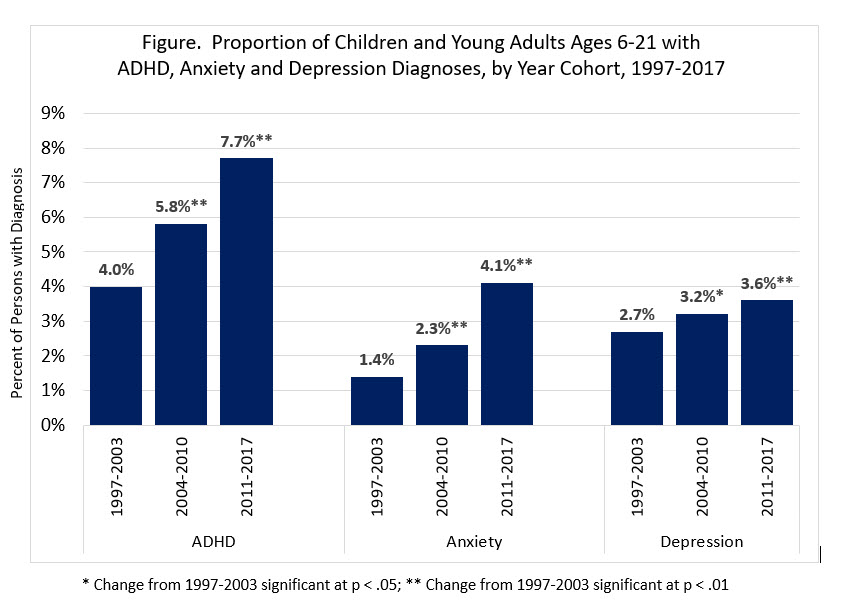
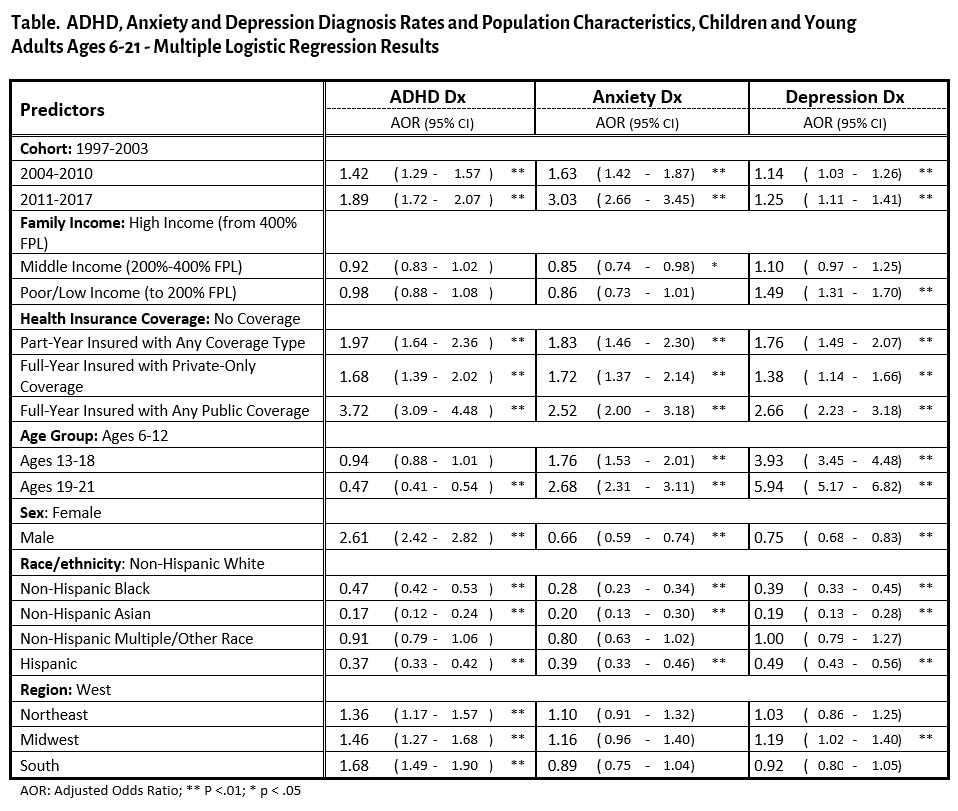
Results: Among US children and young adults, diagnoses for ADHD (4.0% to 7.7%), anxiety (1.4% to 4.1%), and depression (2.7% to 3.6%) increased across the study period (Figure). The differences between the earliest and latest time periods remained significant in multivariable models (ADHD, aOR = 1.89; anxiety, aOR = 3.03; depression, aOR = 1.25) (Table). Diagnoses of all 3 disorders were lower among non-white groups (non-Hispanic black, aOR = 0.28-0.47; non-Hispanic Asian, aOR = 0.17-0.20; Hispanic, aOR = 0.37-0.49) and higher among insured patients (part-year insured, aOR = 1.76-1.97; full-year private, aOR = 1.38-1.72; full-year public, aOR = 2.52-3.72) . ADHD diagnoses were less common for the oldest age group (aOR = .47), and more common for males (aOR = 2.61) and patients outside of the West region (Northeast, aOR = 1.36; Midwest, aOR = 1.46; South, aOR = 1.68). Anxiety and depression, on the other hand, were diagnosed more commonly for the oldest age group (anxiety, aOR = 2.68; depression, aOR = 5.94) and less commonly for males (anxiety, aOR = .66; depression, aOR = .75). Low income was associated with higher depression diagnoses (aOR = 1.49) but middle income was linked to lower anxiety diagnoses (aOR = .85) than high income.
Conclusion: Pediatric ADHD, anxiety and depression diagnosis rates rose between a third to 3 folds over the recent 2 decades and the increases persisted after adjusting for patient factors such as health insurance and income. This suggests that increases in mental health diagnoses are not fully explained by greater access to health care.
Last Updated
10/08/2021
Source
American Academy of Pediatrics