Matthew Kronman, Jeffery Gerber, Robert Grundmeier, Chuan Zhou, Jeffery Robinson, John Heritage, James Stout, Dennis Burges, Ben Hedrick, Louise Warren, Madeleine Shalowitz, Laura P. Shone, Jenny Steffes, Margaret Wright, Alexander Fiks, Rita Mangione-Smith.
Presented at the 2019 Pediatric Academic Societies Annual Meeting.
Background: A third of outpatient antibiotic prescriptions for pediatric acute respiratory tract infections (ARTIs) are inappropriate.
Objective: To evaluate the DART QI program’s effectiveness for reducing overall and second-line outpatient antibiotic prescribing rates for pediatric ARTIs.
Methods: Using a stepped-wedge design, the DART QI program enrolled 57 pediatric clinicians from 18 practices belonging to the AAP Pediatric Research in Office Settings (PROS) Network or the NorthShore University Health System from 12/2016 to 6/2018. Practices were randomized to 1 of 4 wedges determining when the intervention was initiated and provided usual care until then.
Clinicians received 3 program modules over 11 months. Module 1 contained two online tutorials—one on evidence-based antibiotic prescribing and one on communication strategies—and two webinars on the same topics. Modules 2 and 3 contained both individualized antibiotic prescribing feedback reports and booster video vignettes to reinforce communication practices.
Outcomes were assessed using electronic health record data. Visits for acute otitis media (AOM), bronchitis, pharyngitis, sinusitis, and upper respiratory infection (URI) were included. AOM, Group A streptococcal (GAS) pharyngitis, and sinusitis were considered bacterial diagnoses. Eligible visits included care for children 6 months to 10 years-old who had not received antibiotics in the prior 30 days. We used mixed-effects logistic regression to compare overall ARTI antibiotic prescribing rates and second-line antibiotic prescribing rates for bacterial ARTIs during a 1-year baseline period compared to 3 periods occurring after implementation of each program module and a post-intervention period.
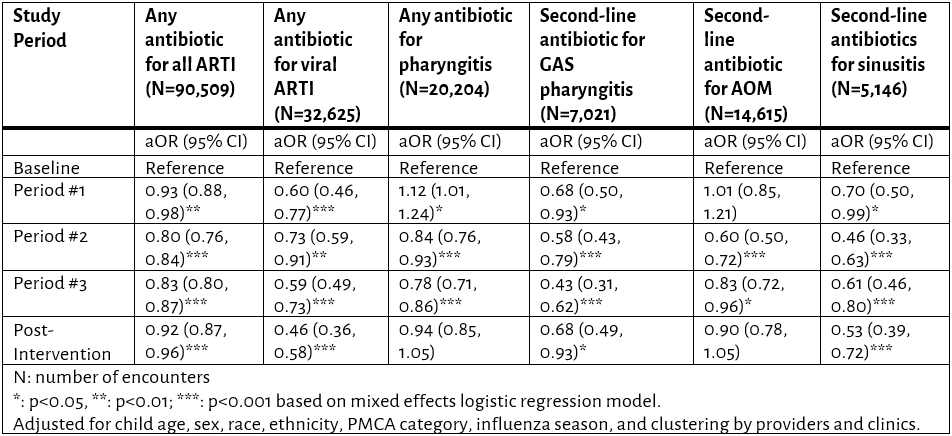
Results: 42 (74%) clinicians completed all three modules. Of 90,509 eligible visits by 31,726 patients (Table 1 below), adjusted intention-to-treat analyses revealed odds of antibiotic prescribing for ARTI overall decreased 8% from baseline to the post-intervention period (Table 2 below), aOR 0.92 [0.87-0.96], corresponding to a mean prescription rate decrease from 42.6% to 38.8% across providers, (Figure 1 below). Odds of second-line prescribing also decreased for GAS pharyngitis (aOR 0.68 [0.49-0.93]) and sinusitis (aOR 0.53 [0.39-0.72]), but not AOM (aOR 0.90 [0.78-1.05]).
Conclusion: The DART QI program reduced inappropriate antibiotic use for outpatient ARTI visits. Extrapolated to national data, this intervention could prevent ~1.5 million inappropriate antibiotic prescriptions annually.
Table 1. Demographic data for all 31,726 included patients.
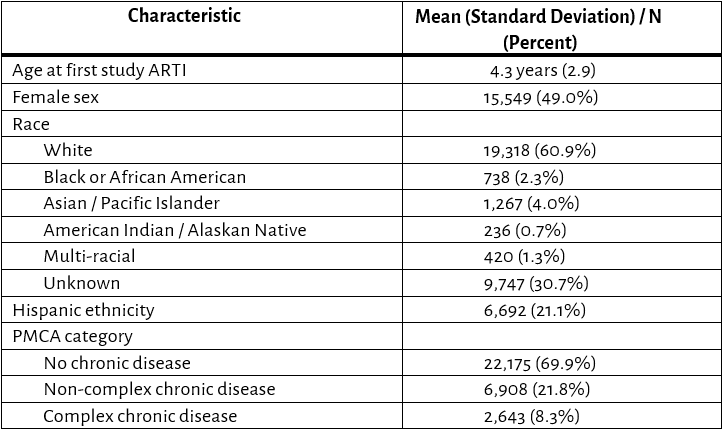
ARTI - Acute respiratory tract infection
PMCA - Pediatric Medical Complexity Algorithm
Table 2. Visit-level Prescribing Rates, by condition
AOM – Acute otitis media
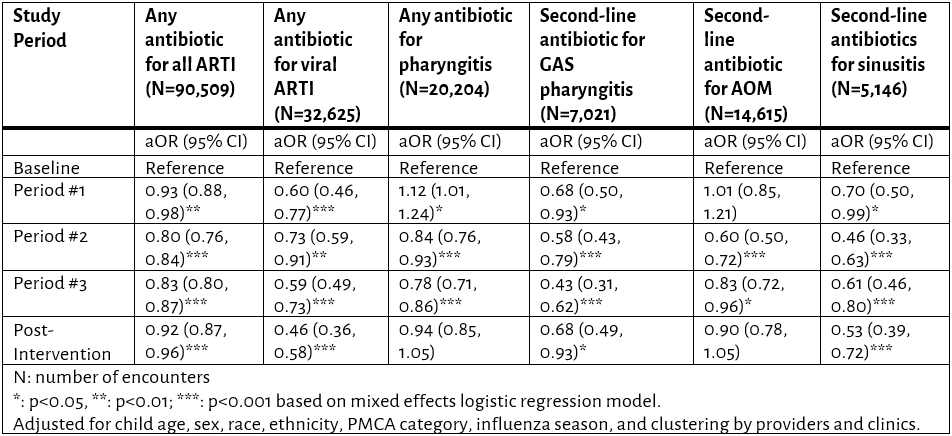
ARTI - Acute respiratory tract infection
GAS - Group A Streptococcus
PMCA - Pediatric Medical Complexity Algorithm
Figure 1. Provider-level Rate of Antibiotic Prescribing for Any Acute Respiratory Tract Infection, by Intervention Period
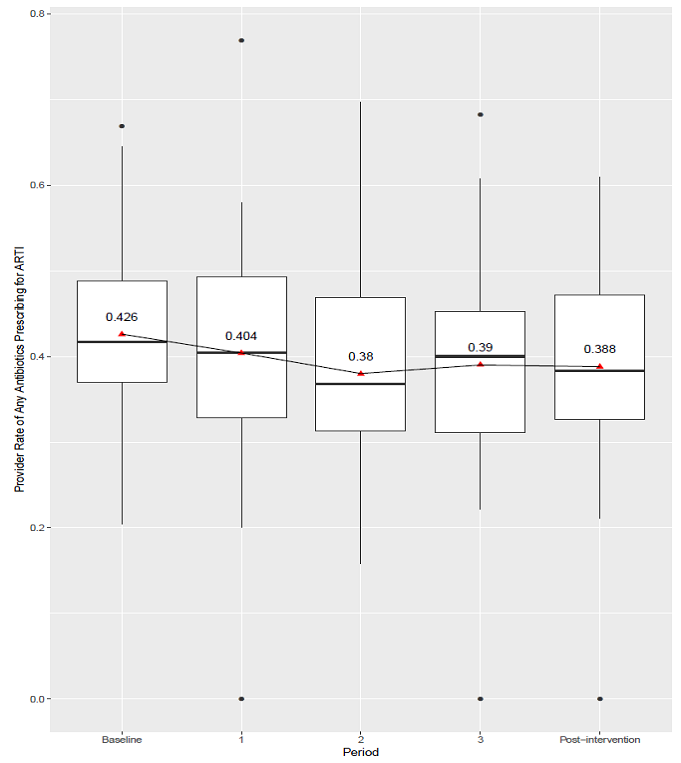
Boxplot indicates median and 25th to 75th percentiles, with outliers represented by filled circles; red triangles represent means.
Last Updated
10/08/2021
Source
American Academy of Pediatrics