Enrollment in High Deductible Health Plans for US Children: Trends, Correlates, and Health Service Utilization and Cost
Kandyce Larson, Elizabeth Gottschlich, Anne Edwards, William Cull, Lynn Olson
Background: High deductible health plans have become increasingly more common among adults, but little is known about children’s enrollment and how this may affect health service utilization and cost to families.
Objective: Examine trends, correlates, and health service utilization and cost for US children with high deductible private health insurance.
Methods: The primary sample includes 16,097 children ages 0-17 with private health insurance from the US National Health Interview Survey (NHIS) 2014-2016 datasets. Trend data on high deductible health plan enrollment are available from 2007-2016 (N=50,326). The NHIS defines high deductible as a minimum of $2,600 for a family or $1,300 for an individual in 2016 (with adjustment for inflation across years). Chi-square tests assess high deductible health plan enrollment by sociodemographic and child health factors. Logistic regression models examine associations between high deductible health plan enrollment and health service utilization and cost adjusted for child age, race, citizenship, family income, education, family structure, global child health status, and disability.
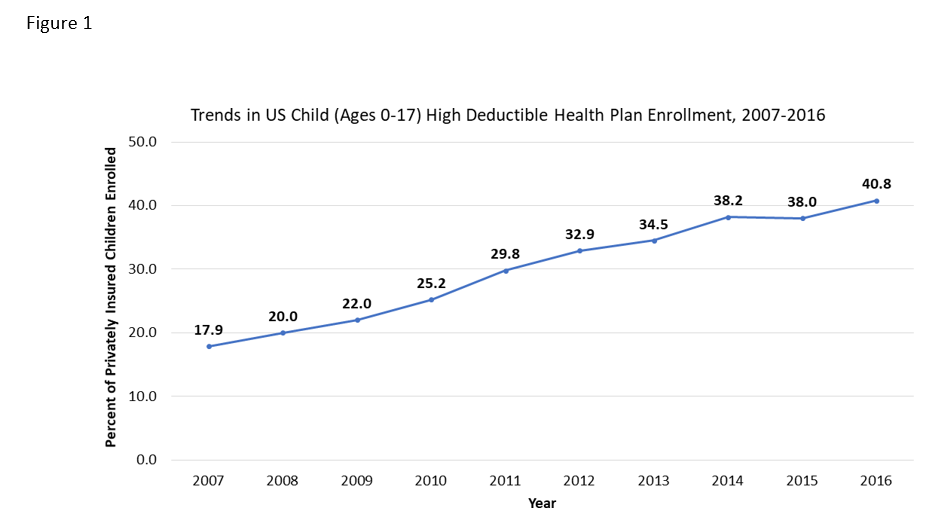
Results: The percent of privately insured children with high deductible plans increased from 18- 41% from 2007-2016 (Figure 1). In 2014-2016, high deductible health plans were more common for white children, US citizens, and those with two parents and higher family incomes and education. For example, 30% of privately insured Hispanic children and 32% of black children had high deductible plans compared to 42% for white children. There were no differences by child age or global health status and disability. In adjusted logistic regression, children in high deductible plans were more likely than those in traditional private plans to have no well-child visit (AOR: 1.17; 95% CI: 1.03-1.34) and no usual source of care (AOR: 1.48; CI: 1.13-1.94), but did not differ for any doctor office visit or a flu shot. Children in high deductible plans also had more unmet health (AOR: 1.96; CI: 1.47-2.62) and delayed medical care (AOR: 2.50; CI: 1.77-3.54) needs, and their families reported more medical debt (AOR: 1.56; CI: 1.42-1.72) and problems paying medical bills (AOR: 1.81; CI: 1.57-2.08).
Conclusion: Privately insured families have seen substantial growth in high deductible health plans in the last decade. Compared to other children with private insurance, those in high deductible plans have less preventive service use and more unaddressed health needs.
Last Updated
10/15/2021
Source
American Academy of Pediatrics