Szilagyi PG, Humiston SG, Breck A, Kelly MK, Wright M, Stephens-Shields AJ, Localio R, Grundmeier RW, Albertin C, Shone LP, Steffes J, Rand CM, Abney DE, McFarland G, Fiks AG
Accepted for 2020 Pediatric Academic Societies Annual Meeting
Background: Low HPV vaccination rates leave many adolescents susceptible to HPV disease. HPV missed opportunities (MOs) are visits at which a patient is eligible for HPV vaccine but does not receive it. Some MOs may be prevented through enhanced clinician communication.
Objective: Evaluate the impact of an online distance-learning communication training intervention for clinicians to reduce MOs for HPV vaccination among 11-17 year-olds. We hypothesized the intervention would reduce MOs, particularly for HPV1 at well-child care (WCC) visits.
Methods: The STOP-HPV trial involved 48 primary care pediatric practices (234 clinicians) in 19 states recruited from AAP's PROS network. We randomly allocated practices to communication training vs. standard of care control. We developed 3 online communication modules to help clinicians (MDs, DOs, nurse practitioners, physician assistants) communicate with parents about HPV vaccine. Topics included: Module 1 (HPV burden, strong clinician recommendation, answering common questions), Module 2 (involving office staff, answering more common questions), and Module 3 (addressing parental hesitancy). We sent weekly text messages to clinicians to reinforce learning goals. We analyzed EHR data to assess (1) HPV MOs by office visit type and HPV dose, and (2) HPV vaccination rates. Analyses were intent-to-treat accounting for clustering by practice.
Results: Altogether 122 clinicians in intervention practices participated in the communication training, and 120, 119, and 116 clinicians completed modules 1, 2 and 3. During the 6-month intervention period, 30,288 adolescents made 24,092 WCC visits and 27,255 acute/chronic visits to intervention practices, and 31,398 adolescents made 24,151 WCC visits and 31,427 acute/chronic visits to control practices.
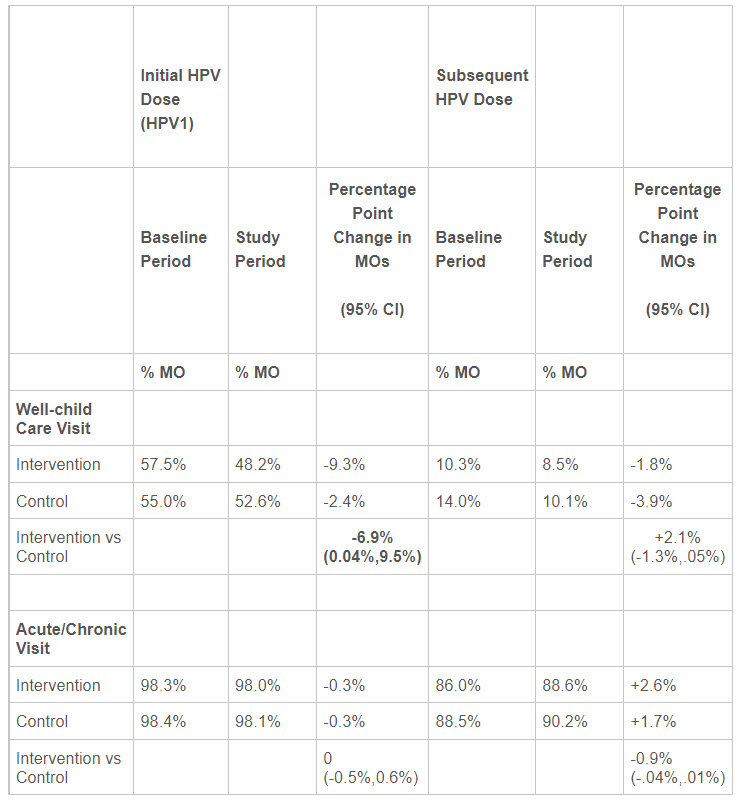
Communication training reduced MOs (unit of analysis is visits, see Table) during WCC visits for HPV1 vaccination by 6.9 percentage points in intervention vs control practices (95% CI 0.04%, 9.5%), but there was no effect of the intervention at acute/chronic visits. Among adolescents (unit of analysis is patient), the change-from-baseline HPV1 vaccination rate was 3.4% better for intervention vs control groups (95% CI= 0.3%, 6.4%).
Conclusions: This potentially scalable, online communication training intervention reduced MOs for initial HPV vaccination at WCC visits and improved HPV1 vaccination rates.
Table: Percent of adolescent office visits at which a Missed Opportunity (MO) for the initial (HPV1) or subsequent HPV dose occurred, for intervention versus control groups, for the baseline and study periods. Note that a reduction in MOs represents an improvement. The unit of analysis is visits.
Last Updated
05/20/2020
Source
American Academy of Pediatrics