Kandyce Larson1, Elizabeth Gottschlich1, Lynn Olson1
1American Academy of Pediatrics, Itasca, IL.
Presented at the 2019 Pediatric Academic Societies Annual Meeting.
Background: Prior studies have shown improvement in insurance coverage for low-income children and a narrowing of disparities for basic access indicators. Less clear is whether income gradients in children's health have also improved.
Objective: Examine income gradients in children's health in parallel with access improvements and determine how the gradients have changed over time.
Design/Methods: This study includes 32,206 children under age 18 from the 2015-17 National Health Interview Surveys and 38,267 children from 2001-03. We used parent report of 12 child health and 6 access to care indicators. For 2015-17, chi-square tests assess associations between family income (<100% Federal Poverty Level (FPL), 100-199% FPL, 200-399% FPL, ≥400% FPL) and health. Adjusted logistic regression models for health outcomes control for child age, gender, race/ethnicity, nativity, family structure, and insurance status. Models for access outcomes exclude insurance status and add overall child health status. To examine disparity trends, data from all years were included and statistical interactions between study period and income were assessed via F-tests in adjusted models and predicted probabilities were calculated.
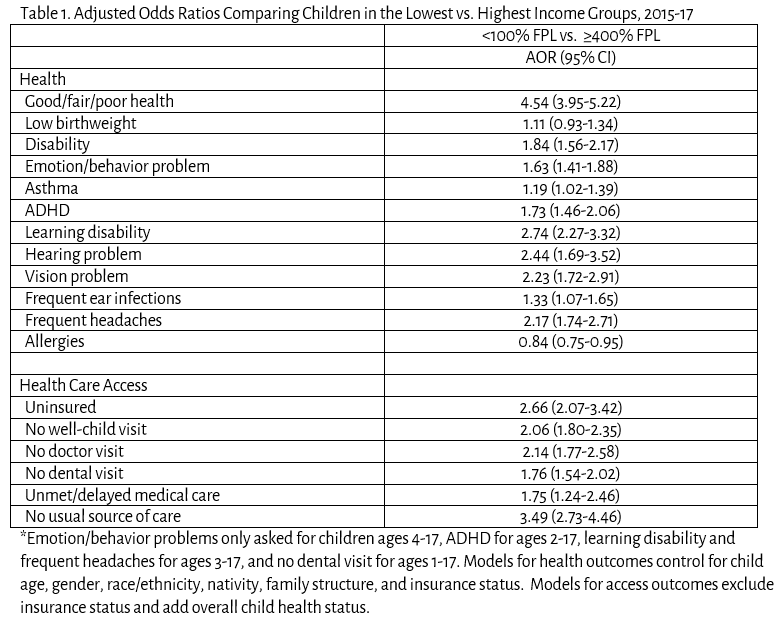
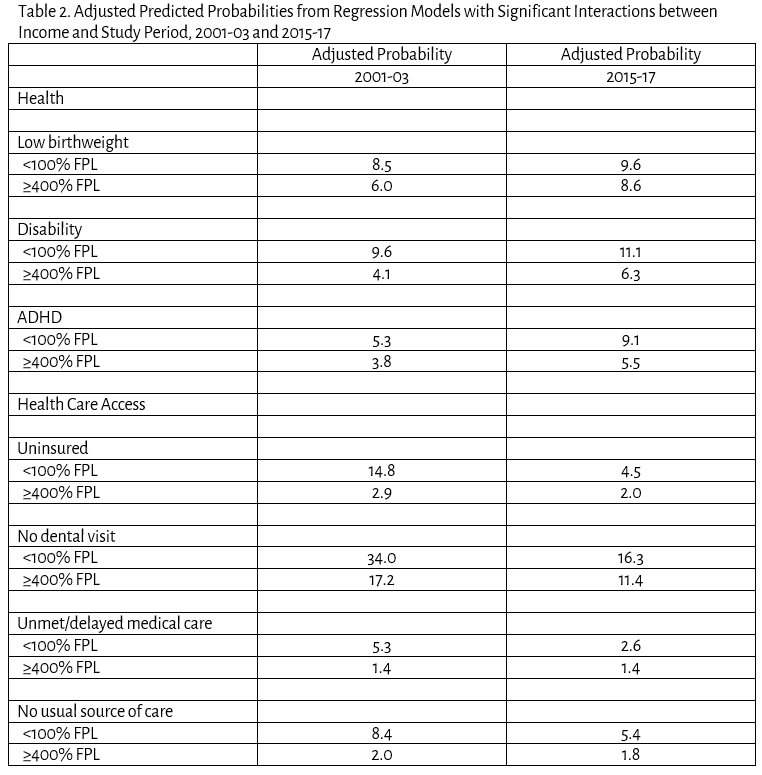
Results: Children with lower family income had worse health and health care access for 17 indicators in 2015-17. In adjusted models, odds ratios >1.5 comparing children in the lowest vs highest income group were found for disability, emotion/behavior problems, ADHD, no dental visit, and unmet/delayed medical care; odds ratios >2 were found for good/fair/poor health, learning disability, hearing problems, vision problems, headaches, and 4 of 6 access indicators (Table 1). For 11 indicators, statistical interactions showed no change in the magnitude of the disparities since 2001-03 (p>.05). Gradients for 1 health outcome widened and 2 narrowed (Table 2). Adjusted predicted probabilities of ADHD increased from 5.3-9.1% for children in poor families vs 3.8-5.5% for the highest income group. Low birthweight and disability increased more for children in the highest income group. Disparities narrowed for 4 of 6 access outcomes. For example, unmet/delayed medical care probabilities decreased from 5.3-2.6% for children in poor families but stayed at 1.4% for the highest income group.
Conclusion: Despite reductions in access disparities, income gradients in children's health have not changed much since early 2000. Comprehensive strategies, including but beyond health care, are needed to address income disparities in children's health.
Last Updated
10/08/2021
Source
American Academy of Pediatrics