Kelly M, Stephens-Shields A, Hannan C, Rand C, Localio R, Shone L, Steffes J, Davis K, Grundmeier R, Albertin C, Humiston S, Abney D, Szilagyi P, Fiks A
Presented at the 2023 Pediatric Academic Societies Annual Meeting
Background: The COVID-19 pandemic disrupted healthcare delivery in pediatric primary care practice, causing many children to fall behind on routine immunizations. Simultaneously, parental vaccine hesitancy may have risen during this time. Such conditions could lead to more vaccination missed opportunities (MOs), office visits when eligible patients do not receive a recommended vaccine.
Objective: To compare the direction and rate of MO change at adolescent well-care visits pre-pandemic (Jan. 2018-Feb. 2020) and during the pandemic (June 2020-Dec. 2021) for three recommended vaccines: human papillomavirus (HPV), for which vaccine hesitancy is high, and quadrivalent meningococcal conjugate vaccine (MenACWY) and tetanus, diphtheria, and acellular pertussis (Tdap), for which hesitancy is low.
Methods: Using an interrupted time series design, we conducted a secondary data analysis of electronic health record data collected as part of the NIH-funded STOP-HPV trial. We analyzed data from 24 pediatric primary care sites in the AAP Pediatric Research in Office Settings (PROS) network who were in the control group an received no intervention. Sites were located across 13 U.S. states and included 16 independent practices and 8 practices belonging to one of two large health systems. We evaluated in-person well-care visits among 11–17-year-old patients pre-pandemic (Jan. 2018-Feb. 2020) and during the pandemic (June 2020-Dec. 2021). We conducted segmented logistic regression, clustered by practice, to estimate risk differences for MOs during the pandemic relative to pre-pandemic trends.
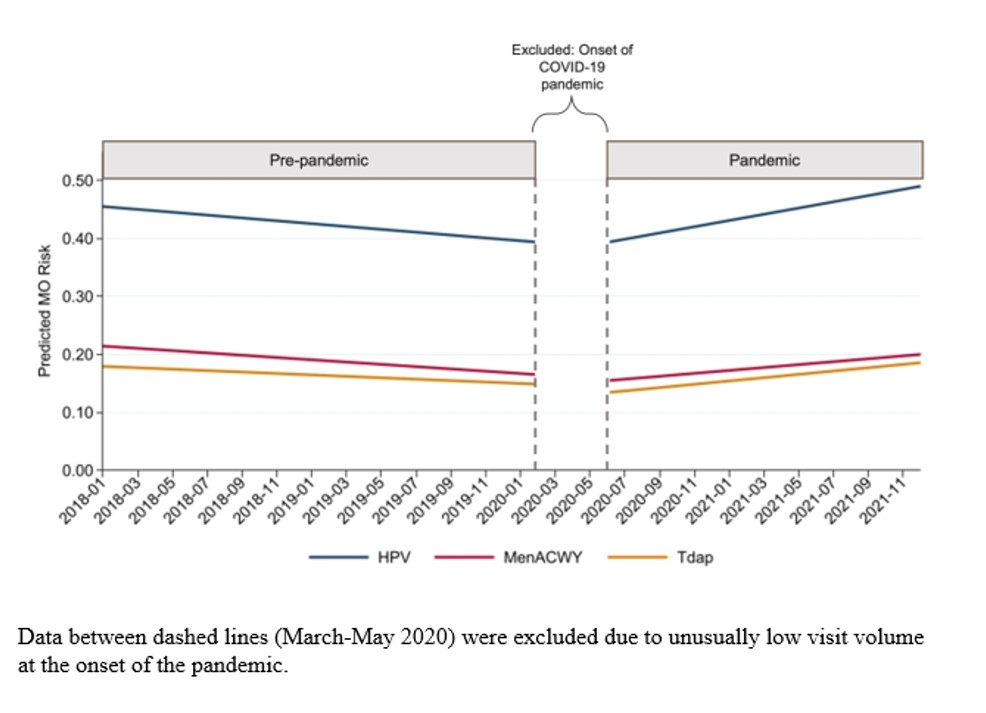
Results: Among 106,605 well-care visits, MOs increased during the pandemic for all three vaccines, but with greater increases for HPV. Relative to pre-pandemic when MO risk was decreasing, MO risk increased significantly for HPV (any dose; +15.9%, 95% CI: 11.7% to 20.1%), MenACWY (either dose; +9.4%, 95% CI: 5.2% to 13.7%), and Tdap (+ 8.2%, 95% CI: 4.3% to 12.1%) (Table, Figure). This pandemic-related increase was larger for HPV compared to MenACWY (+6.5%, 95% CI: 2.8% to 10.3%) and Tdap (+7.7%, 95% CI: 3.1% to 12.3%).
Conclusion: This study demonstrates increasing rates of MOs for three recommended adolescent immunizations during the COVID-19 pandemic through December 2021. Possible explanations include disruptions in staffing and workflow plus increased parental vaccine hesitancy during the pandemic. These findings highlight another impact of the pandemic and the urgent need to reduce vaccine MOs in adolescent well-care to mitigate recent gaps in vaccine coverage.
Table 1. Changes in the risks of missed opportunities for vaccination at well-child care visits before and during the COVID-19 pandemic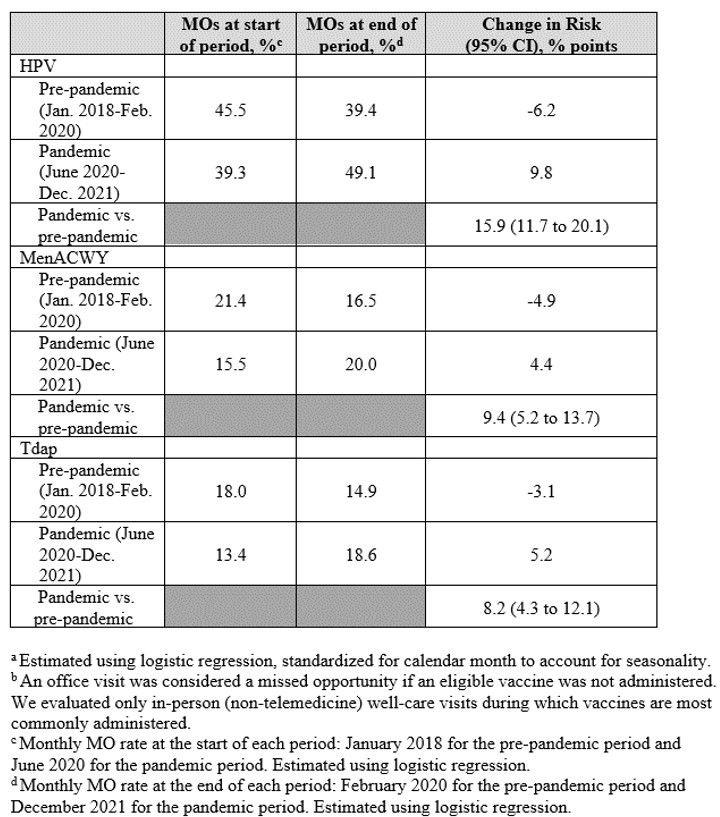
Figure 1. Adolescent vaccine missed opportunities at well-care visits over time
Last Updated
05/22/2023
Source
American Academy of Pediatrics