David C Kaelber1; A.R. Localio2; Michelle Ross2; Janeen B Leon3; Wilson Pace4; Robert Grundmeier5, Jennifer Steffes6, Richard Wasserman7; Alexander Fiks5,6
1Internal Medicine, Pediatrics, Population and Quantitative Health Sciences, and the Center for Clinical Informatics Research and Educations, Case Western Reserve University, Cleveland, OH; 2Biostatistics and Epidemiology, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA; 3Center for Clinical Informatics Research and Education, Case Western Reserve University, Cleveland, OH; 4.American Academy of Family Physicians National Research Network, Denver, CO; Pediatrics, 5Dept of Pediatrics, Perelman School of Medicine at the Univ of Pennsylvania and Children’s Hospital of Philadelphia; Philadelphia PA; 6Pediatric Research in Office Settings, The American Academy of Pediatrics, Itasca IL 7University of Vermont College of Medicine, Burlington, VT; Pediatrics.
Presented at the 2018 Pediatric Academic Societies Annual Meeting.
Background: Currently pediatric hypertension (HTN) is defined as 3 lifetime abnormal blood pressure (BP) measurements. Studies have shown significant under-diagnosis using this definition. Questions remain on how intensively to monitor and intervene in these children.
Objective: To determine the natural history of HTN and pre-HTN in children and adolescents and identify factors associated with risk of persistent HTN and pre-HTN.
Design/Methods: We present a 6-year (72 month) retrospective primary care electronic health record cohort study. We followed blood pressures among 400,000 children at over 2 million visits (51% male; median age
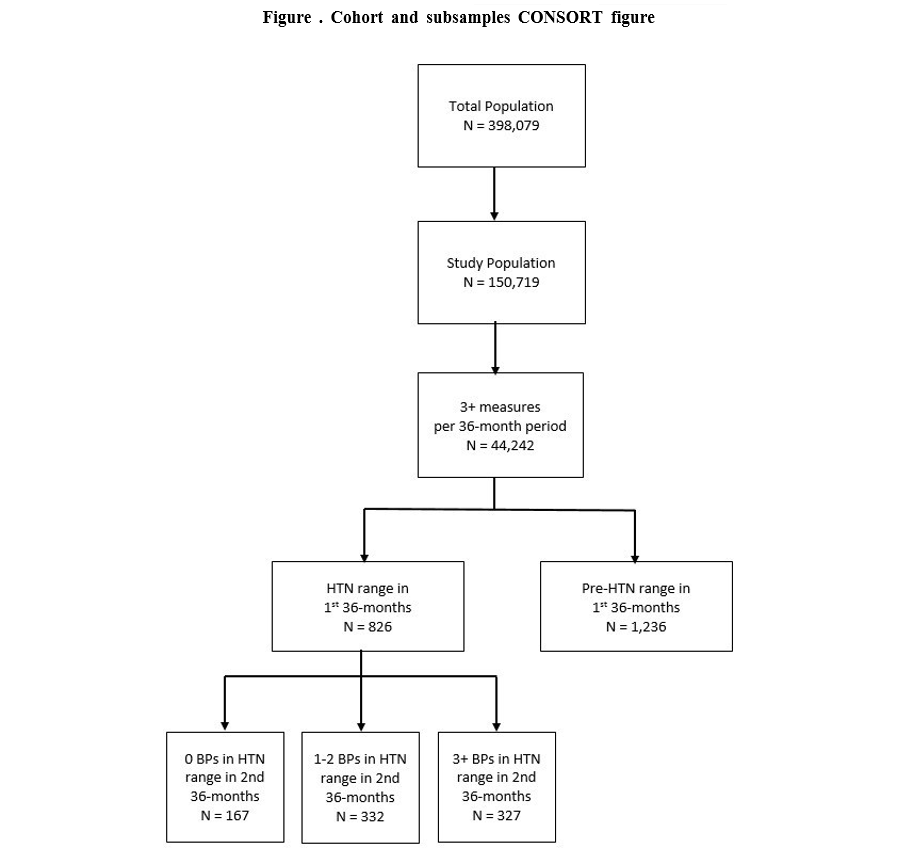
5.25 years and BMI percentile 67.5 at cohort entry; 40% Caucasian, 25% African American, 7% Hispanic; and 32% with public insurance) drawn from 165 sites in 30 healthcare systems. Inclusion criteria included at least 3 BP measurements during each of two 36-month periods (n = 44,242). Observations in the first 36 months (Period 1) were used to predict BP percentile (and BP category) at 72 months (Period 2) using a 3- level mixed effects model. Rates of persistently high BP were tabulated by baseline characteristics.
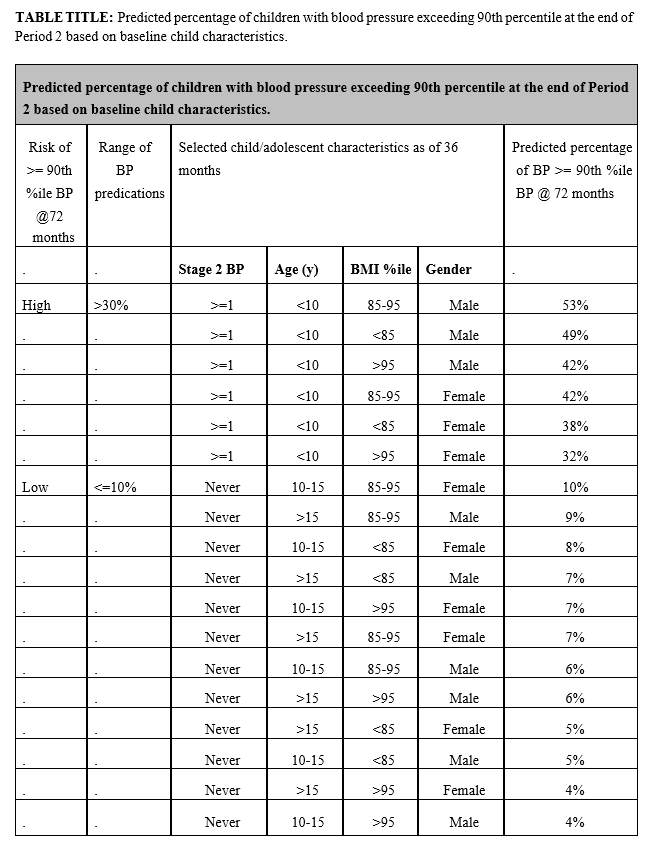
Results: 826 patients met criteria for HTN and 1,236 patients for pre-HTN in Period 1. During Period 2, 167 (20%) of the 826 patients had no BPs in the hypertensive range, 332 (40%) patients had only 1 or 2 elevated BPs, and 327 (40%) of patients had 3 or more BPs in the hypertensive range. Children with one BP in the Stage 2 HTN range at baseline, age <10 years of age, and male gender were at greatest risk (>40%) of predicted blood pressures >90th%ile at the end of Period 2 (see Table). Race/ethnicity, BMI%, insurance type, diagnosis of HTN, and prescription of an anti-hypertensive medications, were not statistically significant factors in the prediction. Of the 1,236 children who had pre-HTN, 872 (71%) did not meet criteria for HTN in period 2, 7.1% had persistent pre-HTN, and 22% developed HTN.
Conclusion(s): In a large cohort of U.S. children from diverse practice settings monitored over a six-year period, we found that most children initially meeting criteria for HTN eventually have subsequent normal BP. Children with certain baseline criteria are more likely to have persistently high BP. These results call into question the validity of a HTN diagnosis based on 3 lifetime in-office BP measurements, and, consistent with current guidelines, indicate the potential value of ambulatory blood pressure monitoring before a formal diagnosis of hypertension is made.
Last Updated
10/15/2021
Source
American Academy of Pediatrics