Margaret Wright, Laura P. Shone, Sharon Humiston, Jenny Steffes, Cynthia M. Rand, Mary Kate Kelly, Abigail Breck, Russell Localio, Alisa J. Stephens-Shields, Robert Grundmeier, Christina Albertin, Dianna Abney, Greta McFarland, Peter G. Szilagyi, Alexander G. Fiks
Presented at the 2019 Pediatric Academic Societies Annual Meeting.
Background: A safe and effective vaccine that prevents HPV-attributable cancers has been available since 2006. Despite demonstrated safety and effectiveness, coverage rates for the HPV vaccine remain suboptimal, and considerably lower than coverage for other adolescent vaccinations.
Objective: Examine a) barriers to HPV vaccination and b) strategies used to improve HPV vaccination rates in a sample of pediatric primary care practitioners from 19 states.
Methods: As part of the NIH-funded STOP HPV trial, the lead practitioner from 47 practices recruited from the PROS research network completed an online, confidential survey in 2018. The survey measured office characteristics, standard office practices for and communication about HPV vaccination, and use of evidence-based strategies such as performance feedback, practitioner prompts, reminder-recall, and standing orders. Proportions and medians were calculated for categorical and continuous variables, respectively.
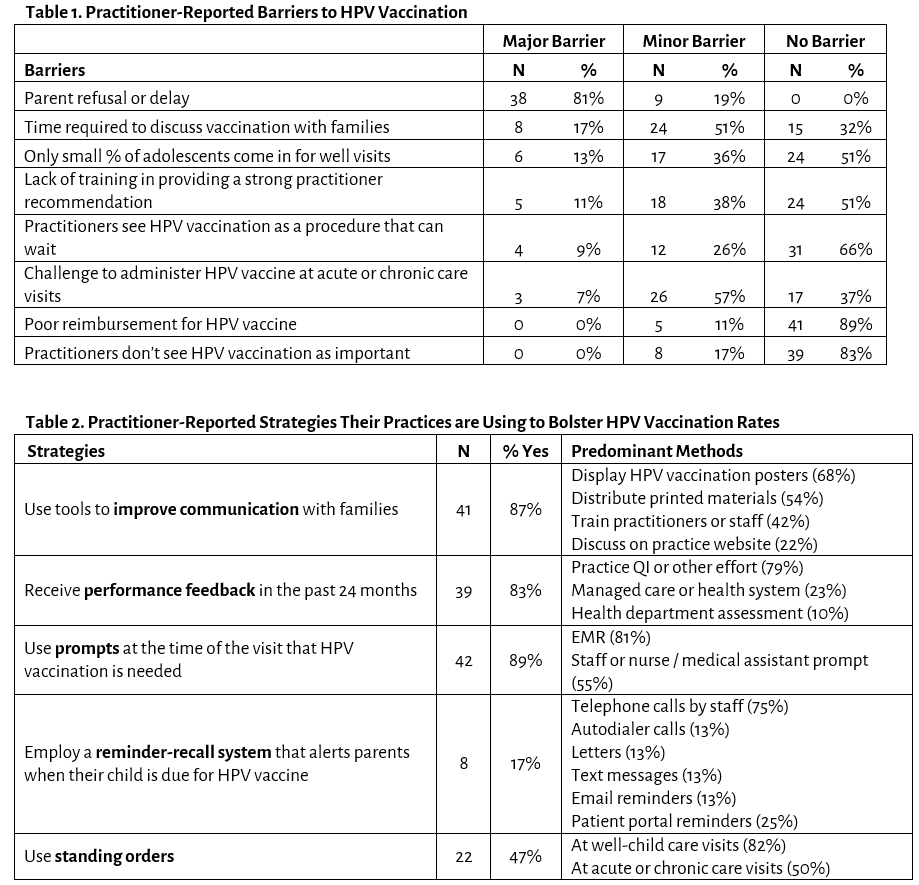
Results: Barriers: All practitioners reported >1 barrier to HPV vaccination. The most commonly reported major barrier was parent refusal or delay (>80%, Table 1). Practitioners reported approximately 30% (range 5%-75%) of parents of their 11-12-year-old patients due for a HPV vaccine refused and 15% (range 5%-60%) hesitated without refusing. Other major barriers reported by practitioners included the time required to discuss HPV vaccination with families (17% of practitioners), low proportion of adolescents coming in for well visits (13%), lack of training in providing a strong practitioner recommendation (11%), practitioners’ view that HPV vaccination can wait (9%), and challenges associated with administering HPV vaccine at acute or chronic care visits (7%).
Strategies The most commonly reported strategy to improve HPV vaccination rates was use of prompts when HPV vaccination is needed (89%, Table 2). Practitioners also reported that their practices commonly use tools to improve communication about HPV vaccination with parents and adolescents (87%) and receive performance feedback about HPV vaccination rates (83%). Only 17% of practitioners cited that their practice uses reminder-recall messages specific to the HPV vaccine. Table 2 provides details about each specific strategy used.
Conclusion: Practitioner-perceived barriers to HPV vaccination persist. Practices are already using a wide variety of strategies to improve delivery of this vaccine, yet room for improvement remains.
Last Updated
10/08/2021
Source
American Academy of Pediatrics