Mary Pat Frintner, MSPH,1 Marybeth Jones, MD, MHPEd,2 Amanda Fisher, MS,1 Janice L. Liebhart, MS,3 Carrie A. Dooyema, MSN, MPH, RN,4 Brook Belay, MD, MPH4
1American Academy of Pediatrics (AAP), Department of Research, Itasca, IL, U.S.; 2University of Rochester Medical Center, Division of General Pediatrics, Rochester, NY, U.S.; 3AAP, Institute for Healthy Childhood Weight, Itasca, IL, U.S.; 4Centers for Disease Control and Prevention, Atlanta, GA, U.S.
Presented at the 2018 Pediatric Academic Societies Annual Meeting.
Background: Pediatricians are on the front lines of addressing childhood obesity and have insights that may help stakeholders understand provider attitudes towards screening, counseling, and current barriers that families face in managing obesity.
Objectives: Assess pediatricians’: a) attitudes towards obesity screening and counseling during well child visits, and b) perceptions of access and financial barriers in obesity-related care.
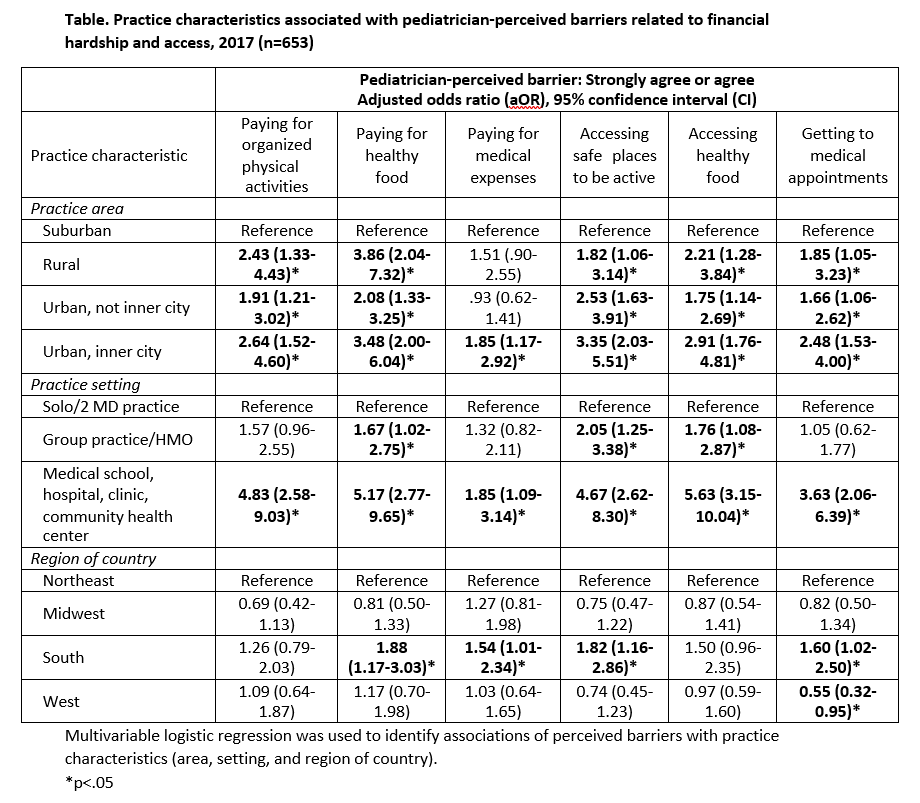
Methods: The Periodic Survey, a national, random sample of AAP US members, focused on obesity in 2017 (response rate=50.1%). Analytic sample included practicing pediatricians and residents who provide health supervision (n=704). Pediatricians were asked about barriers to addressing overweight and obesity at their practice. Multivariable logistic regressions identified associations of perceived barriers with practice characteristics (area, setting, and region of country).
Results: Nearly all respondents agree that pediatricians should address obesity at well child visits (98%). Responses to three separate questions revealed that 61% agree that families want to discuss overweight and obesity, but 22% do not want to offend families by talking about weight and 20% think families are not interested.
The majority perceive that paying for organized physical activities (71%), healthy food (68%), and medical expenses (52%) are barriers for their families. Many perceive that accessing healthy food (59%) and safe places to be active (58%) and difficulty getting to medical appointments (40%) are also barriers.
In multivariable analyses, pediatricians practicing in medical schools, hospitals, and clinics; in urban and rural areas; and in the south, are more likely to perceive access and financial barriers (Table). For example, pediatricians practicing in rural and urban, inner city areas have over 3 times the odds as those working in suburban areas to report that paying for healthy food is a perceived barrier for their families.
Conclusions: Pediatricians self-report that obesity should be addressed at well child visits; 1 in 5 perceive that addressing obesity is not of interest to their families, or will be offensive. Many perceive significant barriers relating to social determinants of health and practice in areas where they perceive patients have suboptimal access to resources for addressing obesity. Enhanced training on engaging with parents about child weight and more collaborations with community interventions to provide resources to address transit, food and activity may be needed.
Last Updated
10/15/2021
Source
American Academy of Pediatrics