Catherine Krafft, MD;1 Mary Pat Frintner, MSPH;2 Alyson B. Goodman, MD, MPH;3 Megan Harrison, MPH, RD;3 Marybeth Jones, MD, MHPEd,1 Janice L. Liebhart, MS;3 Stephen R. Cook, MD, MPH1,4
1University of Rochester Medical Center, Division of General Pediatrics, Rochester, NY, U.S.; 2American
Academy of Pediatrics (AAP), Department of Research, Itasca, IL, U.S.; 3Centers for Disease Control and Prevention, Atlanta, GA, U.S.; 4AAP, Institute for Healthy Childhood Weight, Itasca, IL, U.S.
Presented at the 2018 Pediatric Academic Societies Annual Meeting.
Background: Childhood obesity continues to be a common and complex condition for U.S. pediatricians to address with an estimated 19% of children affected. Studies suggest that MI is effective in bringing about behavior change in children with obesity; however, less is known about pediatrician self-efficacy regarding their ability to use MI effectively.
Objective: To examine characteristics associated with pediatrician-perceived 1) ability to use MI and 2) effectiveness on counseling children with obesity; and, the association between the two.
Methods: The Periodic Survey, a national random sample of AAP U.S. members, focused on obesity in 2017 (response rate=50%). Analytic sample included practicing pediatricians and residents who provide health supervision (n=704). Pediatricians were asked about recent training in MI (last 3 years). Chi- square tests examined pediatrician characteristics and self-rated 1) ability to use MI for behavior change and 2) perceived effectiveness in counseling patients with obesity. Multivariable logistic regression examined ability to use MI and effectiveness in counseling patients with obesity, controlling for age, gender, race/ethnicity, work setting, and region.
Results: Thirty-one percent of all respondents reported recent training in MI. Seventy-one percent reported wanting training; 58% of those recently trained in MI and 79% of those not recently trained in MI reported wanting training in MI.
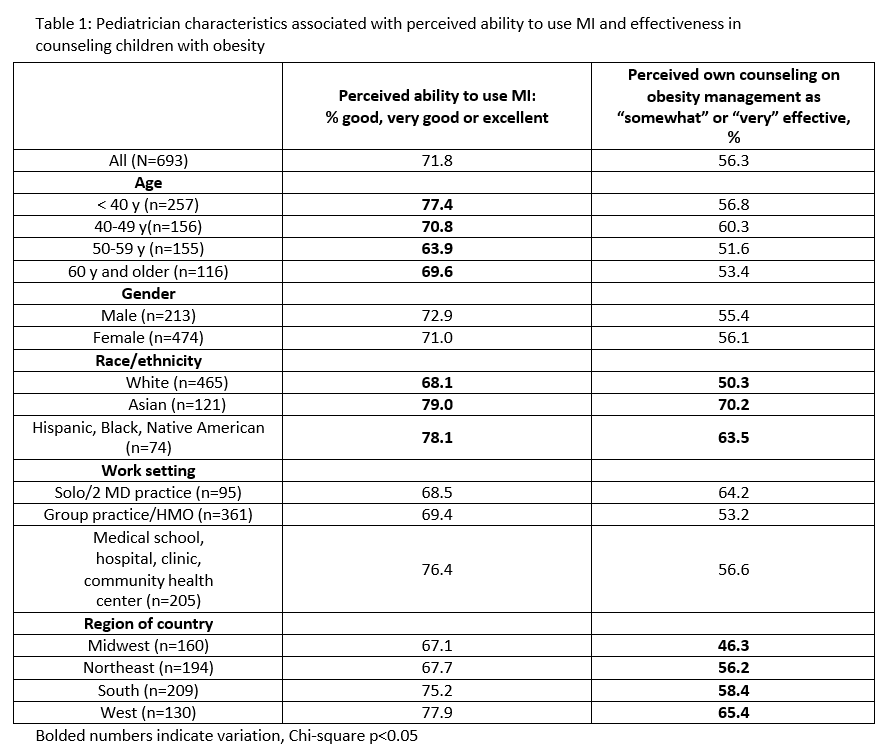
Overall, 72% of respondents rated their ability to use MI as good, very good or excellent. Eight in 10 of those recently trained in MI and 67% of those who were not recently trained reported such ability. Self- rated ability in MI varied by age and race/ethnicity (Table). Over half perceived their own counseling on obesity management as somewhat or very effective, which varied by race/ethnicity and region (Table).
Respondents who rated their ability to use MI as good, very good or excellent were more likely than those rating it as fair or poor to report their counseling on obesity management as somewhat or very effective in both bivariate (67% vs 28%, p<0.001) and multivariable analysis (aOR 4.71, 95% CI 3.20-6.93).
Conclusion: Many pediatrician respondents would like training in MI, and recent training is associated with self-efficacy in MI. Those who feel confident in their MI skills also perceive their counseling of families with children with obesity is effective. These data suggest that national efforts to train pediatricians in MI should continue.
Last Updated
10/15/2021
Source
American Academy of Pediatrics