Sisk, Blake1; Needle, Scott2; Fisher, Margaret3; Houtrow, Amy J.4;Trevathan, Edwin5; O'Leary, Sean T.6
1Research, American Academy of Pediatrics, Itasca, IL, United States.
2Elica Health Centers, Sacramento, CA, United States.
3Monmouth Medical Center, Long Branch, NJ, United States.
4Physical Medicine and Rehabilitation , University of Pittsburgh, Pittsburgh, PA, United States.
5Vanderbilt University Medical Center, Nashville, TN, United States.
6Pediatrics, University of Colorado Anshutz Medical Campus, Aurora , CO, United States
Presented at the 2019 Pediatric Academic Societies Annual Meeting.
Background: Zika virus disease is a nationally notifiable condition in the US. However, little is known about US pediatricians’ experience with screening, treating, and managing patients for Zika.
Objective: To examine pediatricians’ experiences screening, treating, and managing patients for Zika virus.
Methods: Nationally representative 2018 Periodic Survey of American Academy of Pediatrics US members (including primary care physicians and neonatologists). Analysis was restricted to post-residency respondents that provided direct patient care (analytic n=576). Multivariable logistic regression models examined characteristics associated with reporting having ever personally screened or treated a patient for Zika virus (controls: gender, age, specialty, setting, area, region, and hours worked per week).
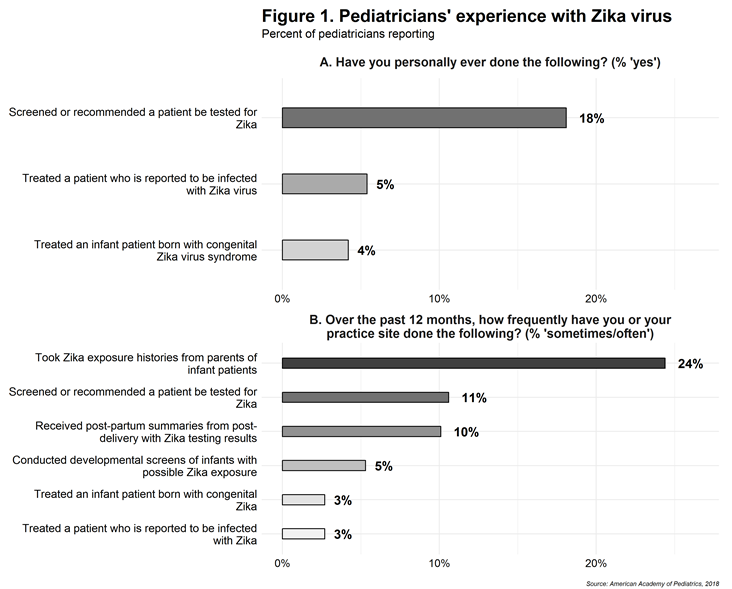
Results: Response rate was 42% (672/1599). There were no differences in response by gender or region, but respondents were somewhat older than non-respondents (46.1 vs 42.2 years). Overall, 18% of pediatricians reported having ever personally screened or recommended a patient be tested for Zika, 5% had treated a Zika-infected patient, and 4% had treated an infant patient born with congenital Zika (Fig 1A). Only 3% of respondents reported that their main practice site sometimes/often treated Zika patients in the past 12 months, 10% reported their practice site received post-partum summaries with Zika testing results, and 5% reported their practice site conducted developmental screens for infants with possible Zika exposure (Fig 1B). Twenty-four percent reported that their practice site took Zika exposure histories in the past 12 months.
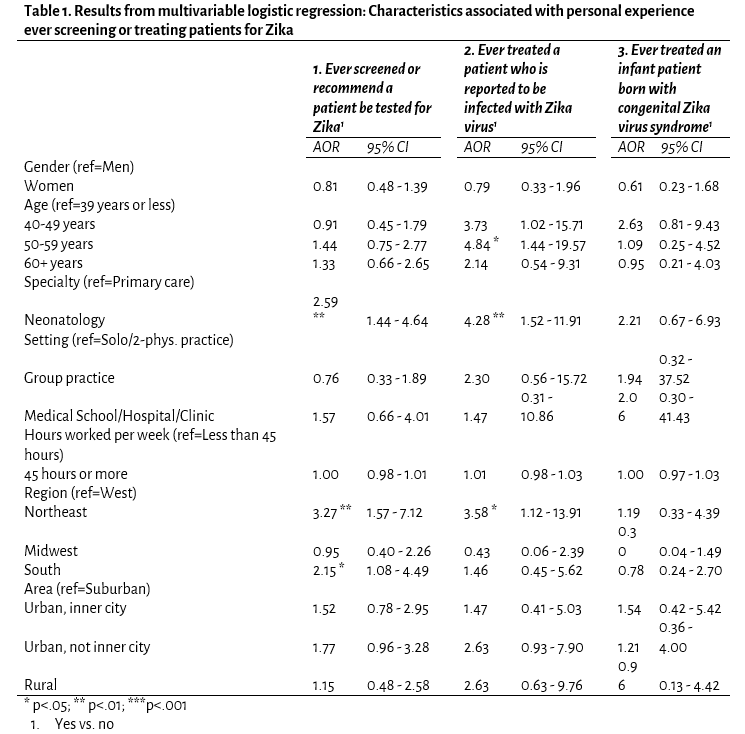
Characteristics associated with having ever personally screened or recommended Zika testing (Table 1) included neonatology subspecialty (AOR=2.59, 95% CI=1.44-4.64) and practicing in the Northeast (3.27, 1.57-7.12) or South (2.15, 1.08-4.49). Similarly, those more likely to report having treated a patient infected with Zika included pediatricians practicing in the Northeast (3.58, 1.12-13.91) and neonatologists (4.28, 1.52-11.91).
Conclusion: Pediatricians’ most commonly reported experience with Zika was taking exposure histories from the families of patients. Overall, relatively few primary care pediatricians or neonatologists have personal experience screening for or treating patients with Zika virus, and this experience is concentrated in the South and Northeast. Given this lack of experience, continued efforts at education of providers on Zika screening will be important going forward.
Last Updated
10/08/2021
Source
American Academy of Pediatrics