Kelly MK, Ramachandran J, Grundmeier R, Wittman S, Macario E, Davis K, Harris D, Steffes J, Biel F, Hatch B, Ray KN, Fiks AG
Presented at the 2025 Pediatric Academic Societies Annual Meeting
Background: According to the National Committee for Quality Assurance’s HEDIS measures, children initiating attention-deficit/hyperactivity disorder (ADHD) medication should be seen for follow-up within 30 days. Telemedicine (TM) could reduce barriers to follow-up and has shown promise for improved ADHD management in research settings. We lack data on widespread impact of primary care TM on this quality measure.
Objective: To assess the impact of TM use for ADHD visits among 6- through 12-year-old children on timely follow-up after ADHD medication initiation in a broad sample of primary care practices.
Methods: Using a retrospective repeated cross-sectional design, we analyzed the electronic health record data of 6- to 12-year-old children who received primary care for ADHD between 2020 and 2023. We evaluated data from 685 Federally Qualified Health Centers, 76 practices from 2 regional health systems, and 38 independent practices from the AAP Pediatric Research in Offices Settings network. We included visits associated with an ADHD diagnostic code (ICD-10 F90.*). We first described the proportion of ADHD visits each year conducted via TM, identified using billing code modifiers (95, GT) and place of service codes (02, 10). Focusing on ADHD visits during which medication was initiated, we examined the association between modality of care (in-person vs. telemedicine) and rates of follow-up visits after ADHD medication initiation using chi-square tests. We defined modality of care based on whether a child had ever received ADHD care via TM at the time of medication initiation. We evaluated follow-up care within 30 days (in accordance with the HEDIS measure) and 42 days (sensitivity analysis reflecting the challenge of 30-day follow-up in practice).
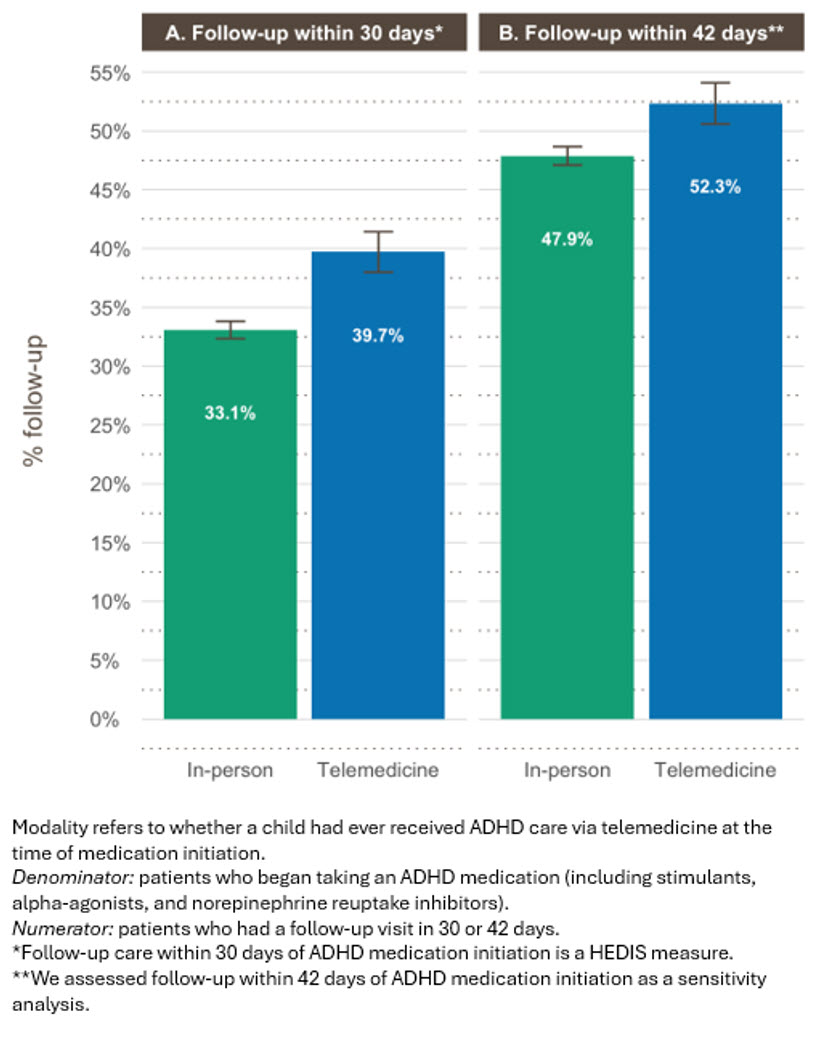
Results: We analyzed 240,357 ADHD visits (19.4% via TM). ADHD visits completed through TM peaked at 31.7% in 2020 before gradually declining to 12.2% in 2023 (Figure 1). Children initiated ADHD medication at 18,749 visits (7.8% of total ADHD visits). Among these children, prior TM use was associated with a 6.6 percentage point greater follow-up rate at 30 days (39.7% vs 33.1%, 95% CI: 4.8% - 8.5%, p<0.001) and a 4.5 percentage point greater follow-up rate at 42 days (52.3% vs 47.9%, 95% CI: 2.5% - 6.4%, p<0.001) (Figure 2).
Conclusion: In this secondary data analysis including 799 primary care practices across the US, TM care for ADHD was associated with greater follow-up rates after ADHD medication initiation among 6- to 12-year-old primary care patients, suggesting that TM may increase the quality of ADHD care.
Figure 1. Percentage of ADHD visits conducted via telemedicine.
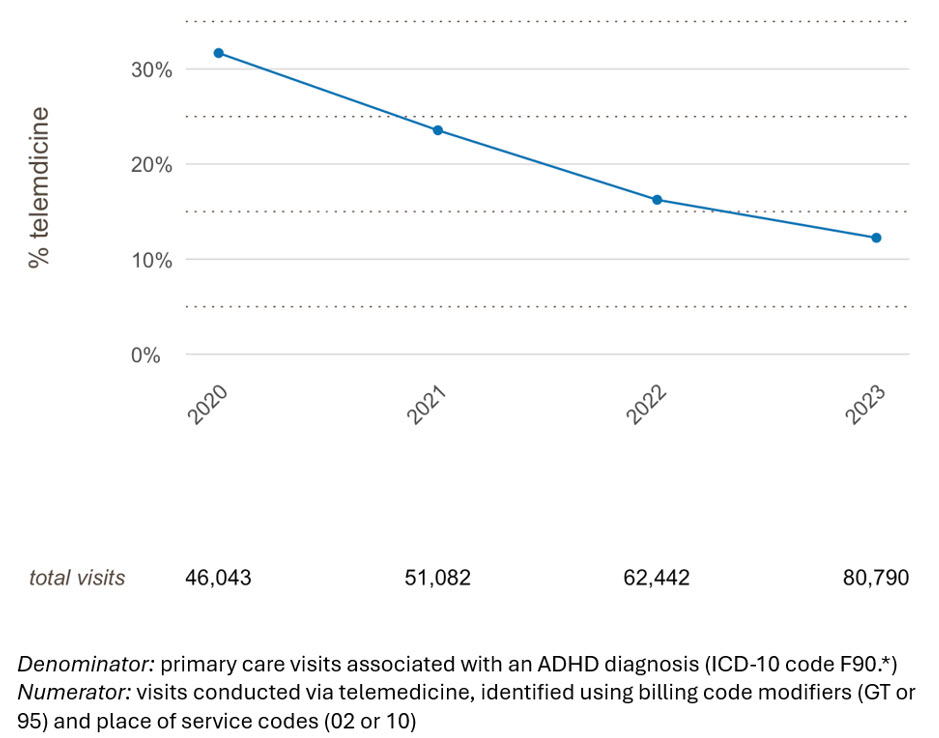
Figure 2. Follow-up after ADHD medication initiation by modality of ADHD care
Last Updated
05/15/2025
Source
American Academy of Pediatrics