Ramachandran J, Kelly MK, Wittman S, Davis K, Harris D, Steffes J, Biel F, Macario E, Mendez D, Hatch B, Grundmeier R, Ray KN, Fiks AG
Presented at the 2025 Pediatric Academic Societies Annual Meeting
Background: With the rapid adoption of telemedicine (TM) in 2020, concerns were raised about inequitable access to TM. TM has the potential to overcome geographic barriers to primary care for children, but lack of device ownership or internet access, and non-English language may limit use. Understanding evolving TM use in primary care for children by demographic characteristics may inform strategies for equitable TM.
Objective:To describe TM users among children in Federally Qualified Health Centers (FQHC), health system affiliated, and independent primary care practices, overall and by child demographics.
Methods: Our retrospective cohort study used electronic health record (EHR) data of primary care patients aged <19 years, receiving health care from 2020-2023 at 774 FQHCs, 76 practices from 2 regional health systems, and 38 independent practices from the AAP-Pediatric Research in Office Settings (PROS) network. TM visits were identified using billing codes (modifiers GT, 95) and Place of Service codes (02, 10). We described the proportion of patients who had any TM visits in each quarter from 2020-2023. We evaluated patterns in TM use across race and ethnicity, rurality (Rural-Urban Commuting Area (RUCA) codes), household primary language, and payer, as recorded in the EHR.
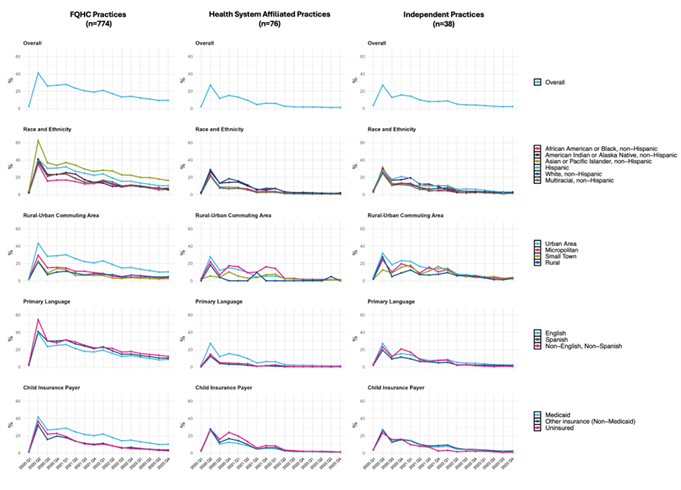
Results: Our cohort included 1,998,637 children (29.3% Hispanic, 83.2% from urban areas, 18.3% Spanish primary language, 62.8% Medicaid insured) who received care at participating sites from 2020 and 2023 (Table 1). The percentage of patients who had at least one TM visit decreased from 31.1% in Q2 2020 to 5.2% in Q4 2023 (Fig 1). In Q1-Q4 2023, TM use by quarter was highest for FQHCs (10.5%), within which TM use was higher for Asian or Pacific Islander children (18.5% v 11.6% Hispanic v 7.2% Black), urban area children (11.4% v 4.9% rural), children of households speaking languages other than English or Spanish (13.9% v 11.4% Spanish and 9.5% English), and Medicaid-insured children (11.3% v 4.3% other insurance). In contrast to FQHCs, TM use was lower for health system affiliated (1.5%) and independent practices (2.6%), with less variation in TM use across child demographics in these settings by Q4 2023 (Fig 2).
Conclusion: While primary care TM use among children declined from 2020 to 2023, we found that FQHCs had the highest TM use in 2023, and greater use among Asian or Pacific Islander children, non-English speakers, and Medicaid insured. Understanding structures that drive these patterns may offer insights to promote equitable TM use in primary care.
Table 1. Demographic characteristics of children with any primary care visits at 888 health centers between 2020 and 2023
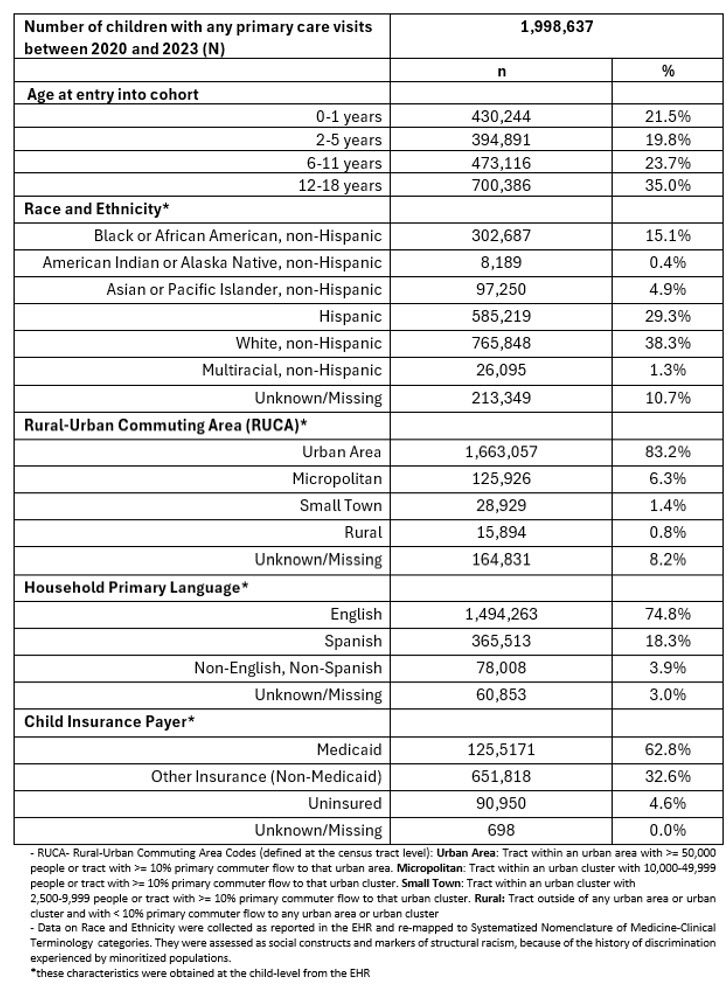
Figure 1. Percentage of primary care patients who had any telemedicine visits in each quarter at 888 health centers from 2020-2023
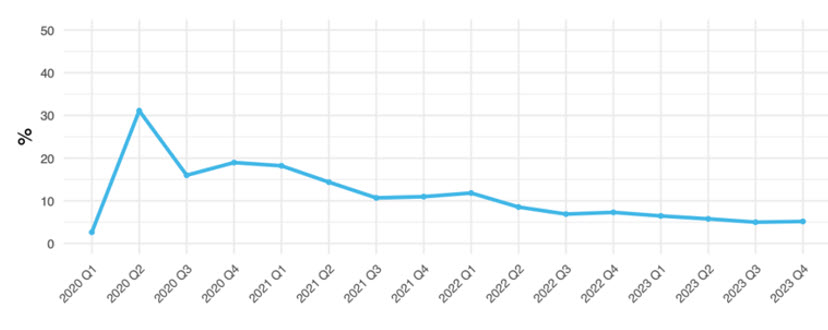
Figure 2. Percentage of primary care patients who had any telemedicine visits in each quarter from 2020-2023, by practice type and demographic characteristics
Last Updated
05/15/2025
Source
American Academy of Pediatrics