Barahona Paz K, Tyrrell H, Brochier A, Griffith M, Joiner T, Scheinlin B, Serwint J, Stockwell M, Torres A, Zelinksy J, Tripodis Y, Garg A
Presented at the 2023 Pediatric Academic Societies Annual Meeting
Background: Identifying families’ unmet social needs and referring them to community resources is becoming standard practice in pediatric primary care. However, little is known about predictors associated with parents’ acceptance of resources.
Objective: To assess the association between child, parent, household, practice-level characteristics and contact mode with parental acceptance of resources.
Methods: We used data from the control arm of a NIH funded clinical stepped-wedge trial, testing the implementation and effectiveness of the WE CARE social care model. Through the Academic Pediatric Association’s Continuity Research Network and the American Academy of Pediatrics’ Pediatric Research in Outpatient Settings network, 18 practices across 14 states participated in the trial (8 urban, 6 suburban, and 4 rural regions). Overall, 1,054 parents (51.8% of approached) of children aged 2 months to 10 years old enrolled from 12/2019 to 5/2022. Participants completed an index survey to assess six social risks (childcare, parent education, parent employment, food, housing, utilities) and sociodemographic and household characteristics. Parents completed a follow-up survey three months later and the research team offered information sheets listing resources. Using logistic regression with only significant variables from bivariate analysis (p<0.05), we assessed predictors of parents’ acceptance of resources.
Results: Overall, 35.1% (n=241) of parents accepted resources for unmet needs. Acceptance rates were 42% in urban, 31% in rural, and 29% in suburban practices (p=.05). We found significant predictors of resource acceptance at multiple levels (Table 1): Child: children with special healthcare needs (aOR 1.7, 95%CI 1.1-2.6); or commercial insurance (aOR 1.9, 95%CI 1.1-3.2). Parent: not married, never married, or separated (aOR 4.8, 95%CI 1.8-13). Household: having one or two parents employed; household food insecurity. Practice: parents attending Northeast (aOR 6.7, 95%CI 2.5-18) and Southwest practices (aOR 2.7, 95%CI 1.2-6.1); presence of social worker. Contact mode: email (aOR 0.4, 95%CI 0.3-0.7) or text (aOR 0.6, 95%CI 0.3-0.9) communication had lower odds of acceptance of resources vs. telephone.
Conclusion: Over one-third of parents from diverse pediatric practice settings in the US accepted resources for unmet social needs offered by research staff. We found important predictors of parental acceptance of resources that, if ultimately similar, might have implications when practices offer resources that mitigate families' unmet needs.
Table 1. Child-, parent-, household-, practice-level characteristics and contact mode by parents who accepted resources and those who did not.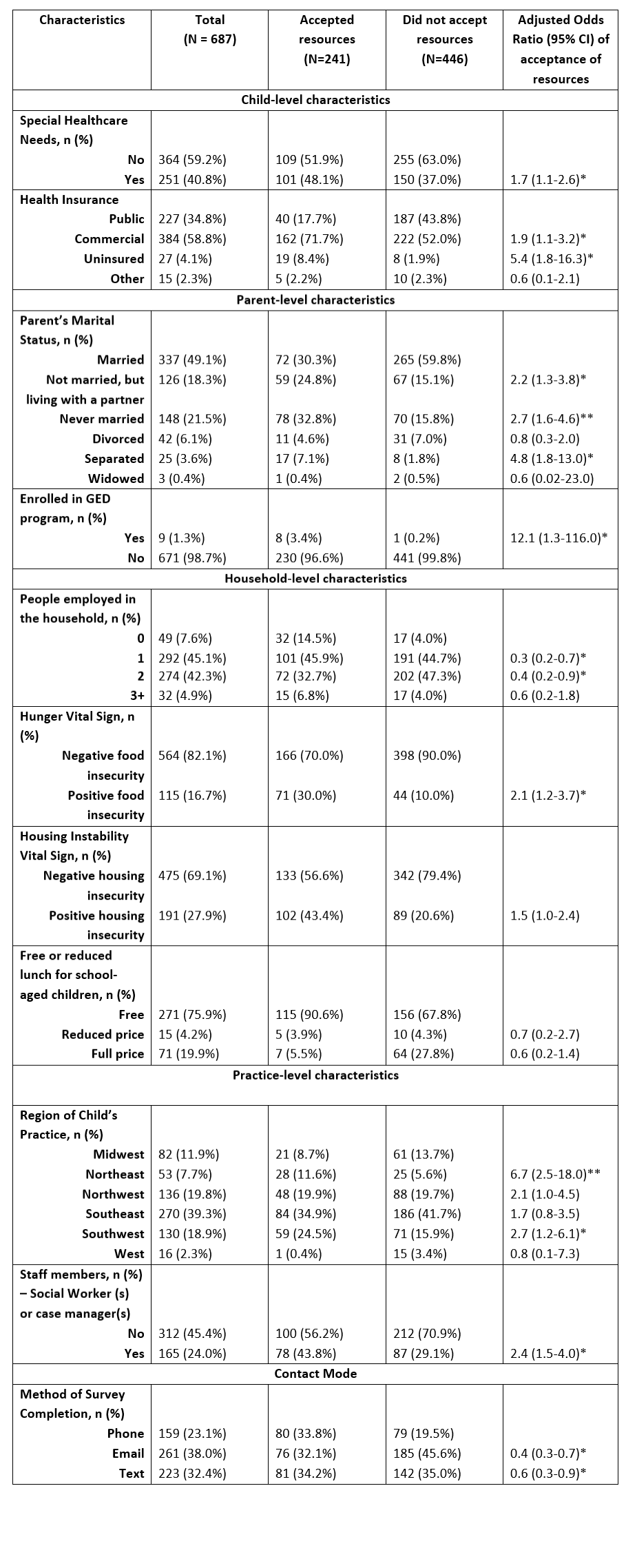
Last Updated
05/22/2023
Source
American Academy of Pediatrics