Stephen R. Cook, MD, MPH,1,2 Mary Pat Frintner, MSPH,3, Janice L. Liebhart, MS,1 Jeanne Lindros, MPH,1 Megan Harrison, MPH, RD,4 Brook Belay, MD, MPH,4 Blake Sisk, PhD,3 Sandra G. Hassink, MD, MS1
1American Academy of Pediatrics (AAP), Institute for Healthy Childhood Weight, Itasca, IL, U.S.; 2University of Rochester Medical Center, Rochester, NY, U.S.; 3AAP, Department of Research, Itasca, IL, U.S.; 4Centers for Disease Control and Prevention, Atlanta, GA, U.S.
Presented at the 2018 Pediatric Academic Societies Annual Meeting.
Background: During the past decade, attention has focused on obesity assessment and prevention, as well as educational curricula and clinical tools to address obesity in pediatric primary care.
Objectives: To examine findings from national American Academy of Pediatrics (AAP) surveys about pediatricians’ practices and attitudes regarding obesity assessment, prevention, and treatment in children 2 years and older.
Methods: The Periodic Survey of a national, random sample of AAP U.S. members focused on obesity in 2006, 2010 and 2017; response rates were 63% (n=677), 58% (n=743) and 50% (n=704), respectively.
The analytic sample included practicing pediatricians (non-residents) who provide health supervision. Bivariate analyses examined BMI assessment across 3 surveys, and discussion of healthy behaviors with families and practice attitudes in the 2006 and 2017 surveys. Multivariable logistic regression examined the independent association of survey year with) BMI assessment, b) discussions of healthy behaviors, and c) attitudes and practices related to obesity; age, gender, hours/week worked, practice area and setting were controlled.
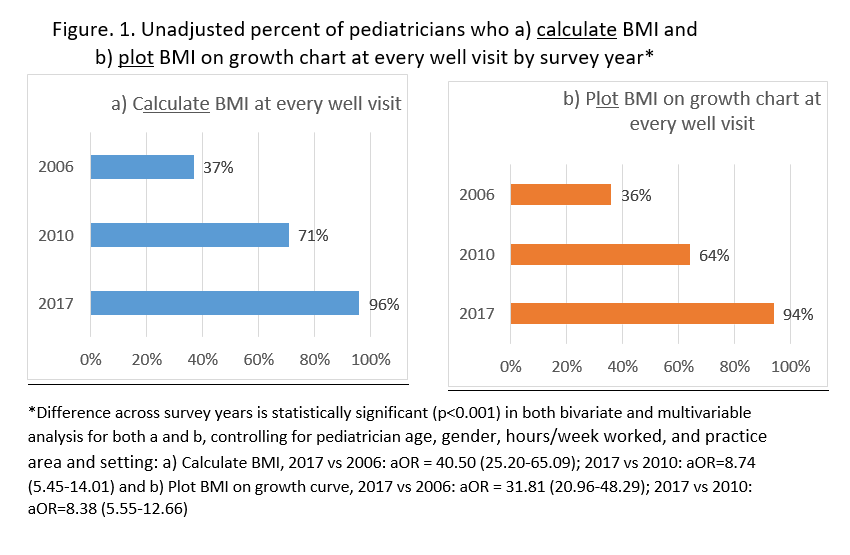
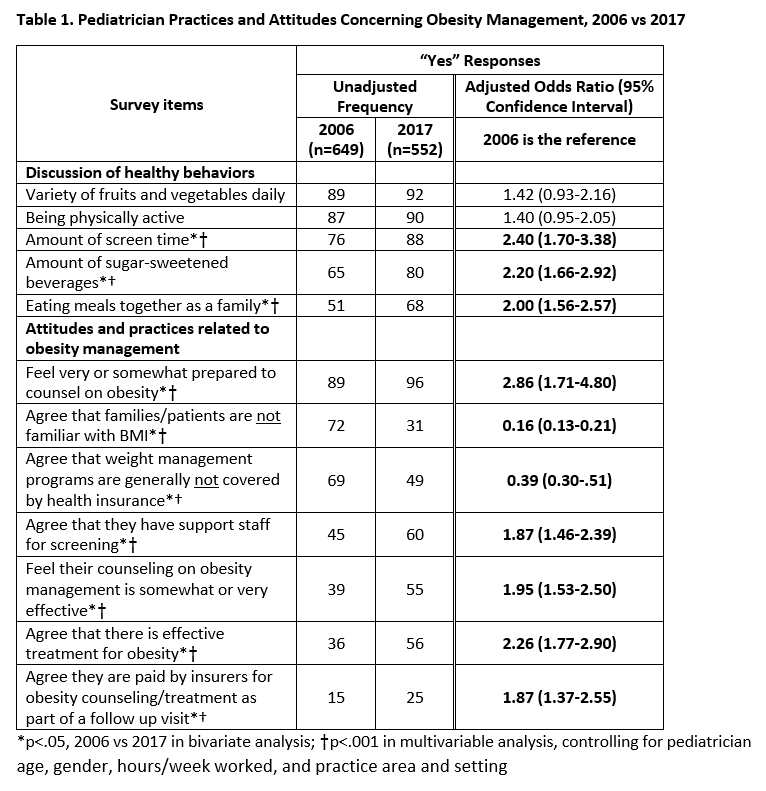
Results: Pediatricians in 2017 were significantly more likely than in 2006 and 2010 to report calculating and plotting BMI at every well-child visit, p<.001 [Figure 1]. Compared to 2006, in 2017 respondents were more likely to discuss family behaviors related to screen time, sugar-sweetened beverages, and eating meals together as a family (Table). Pediatricians in 2017 were also more likely to agree they have staff support for screening, and less likely to agree that families and patients are not familiar with BMI (Table). Pediatricians in 2017 had higher odds of agreeing that there is effective treatment for obesity (aOR 2.26, 95% CI 1.77-2.90), they are well prepared to counsel on obesity (aOR 2.86, 95% CI 1.71-4.80), and their counseling on obesity management is effective (aOR 1.95, 95% CI 1.53-2.50).; they also had higher odds with agreement that follow-up visits for obesity counseling/treatment were paid for (aOR 1.87, 95% CI 1.37-2.55).
Conclusions: Nationwide, practicing pediatricians since 2006 have significantly increased BMI assessments. Providers’ awareness, behaviors and practice around obesity have also improved significantly since release of national guidelines in 2007. Continued support on training and dissemination of practice guidelines will be needed to sustain this progress.
Last Updated
10/15/2021
Source
American Academy of Pediatrics