Bobbi Byrne1, Mary Pat Frintner2, Amy Starmer3, Gary Freed4
1Department of Pediatrics, Indiana University, Indianapolis, Indiana; 2American Academy of Pediatrics, Itasca, IL; 3Department of Pediatrics, Tufts Medical Center Floating Hospital for Children, Boston, Massachusetts; 4Department of Pediatrics and Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, Michigan.
Presented at the 2019 Pediatric Academic Societies Annual Meeting.
Background: Literature suggest that physicians experience burnout at higher rates than the general population, however defining "burnout" is inconsistent. Though the Maslach Burnout Inventory (MBI) is considered the leading measure, its length and cost has led researchers to use alternate ways to assess burnout.
Objective: We aimed to assess how different measurement approaches might result in varying levels of reported burnout, using 2 domains typically considered: emotional exhaustion (EE) and depersonalization (DP).
Methods: National data from the AAP Pediatrician Life and Career Experience Study (PLACES), a longitudinal study of early to mid-career pediatricians were used to examine self-reported burnout. In a 2017 survey, respondents were randomly assigned to 3 alternative ways to assess burnout: 1) MBI (burnout defined as scoring high: >27 on EE and/or >10 on DP scales); 2) simple 2-item measure (burnout defined as agreeing with items on EE and/or DP); and 3) new questions, purposefully designed to measure a more severe level of burnout (defined as at least weekly on EE and/or DP items). Repeated measures logistic regression compared different ways to classify burnout (EE or DP vs EE and DP) and examined alternative questions on burnout.
Results: 71% of participants completed the surveys (1279/1800) with no significant difference in response rate or baseline burnout (measured earlier in 2017).
For participants completing the MBI, 45% were considered burned out based on the EE or DP classification, whereas 15% were considered burned out using EE and DP (Table). For participants completing the simple 2-item measure, 50% agreed they often felt emotionally exhausted at work (EE) or felt less sensitive to patients' feelings (DP), only 19% agreed with BOTH. For participants completing new burnout questions, 14% reported being emotionally exhausted and distressed with nothing else to give at least weekly (EE) or disconnected or cynical towards patients at least weekly (DP) but only 5% reported feeling BOTH at least weekly. For all 3 ways, burnout is significantly higher when classified as EE or DP than when classified as EE and DP, p<.001. Percent reporting burnout based on new burnout questions was significantly lower than the other 2 ways, p<.001.
Conclusion: Burnout is a hot topic in medicine and different methods of measurement yield different results regarding its prevalence and severity. Rates of burnout vary greatly by how questions on burnout are phrased and conceptualized. Regardless of measurement, conceptualization of EE and DP must be considered.
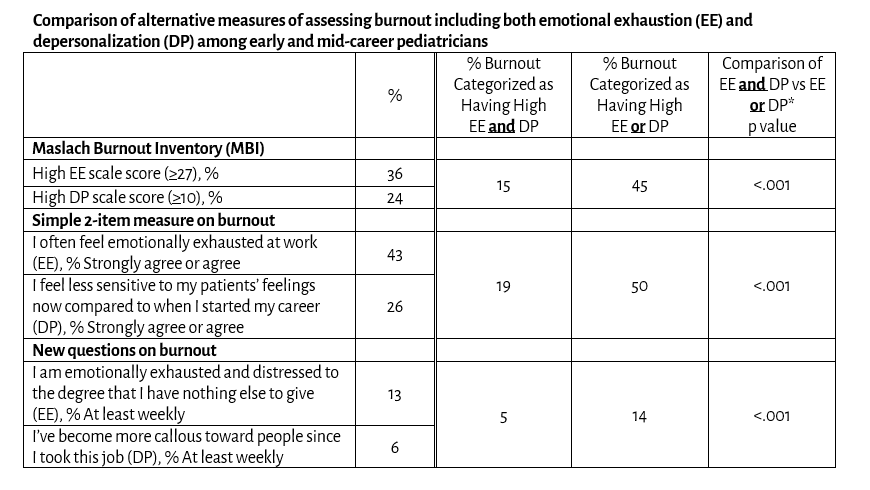 *Repeated measures logistic regression compared EE or DP with EE and DP (within-subjects comparisons)
*Repeated measures logistic regression compared EE or DP with EE and DP (within-subjects comparisons)