The culture of the medical profession has been recognized as a key deterrent in physicians caring for themselves. Research suggests physicians tend to neglect physical examinations and delay seeking medical treatment for themselves. Long shift hours and resulting fatigue contribute to negative personal and professional consequences. For example, physicians who report burnout are also more likely to have increased number of medical errors, malpractice suits, incidence of substance abuse, car crashes and family discord (Factors Related to Physician Burnout 2018 Behav Sci).
Taking care of yourself should be a priority not only because it affects the quality of care you can offer children and their families but because it supports your ability to thrive in medicine and cultivate joy in life.
Emotional Intelligence and Resilience
Emotional Intelligence (EI) is “an ability to recognize the meanings of emotions and their relationships, and to reason and problem-solve on the basis of them.” (Mayer, 1999). Being able to regulate one’s emotional response can be important in controlling or minimizing stress and subsequent burnout. In professions outside of health care, emotional intelligence has been shown to be related to increased productivity, job satisfaction and academic success. Studies have found, higher emotional intelligence was positively associated with more compassionate and empathetic patient care, more effective coping of pressure and leadership, and improved teamwork. (Laura-Elena Năstasă and Anca Daniela Fărcaş / Procedia - Social and Behavioral Sciences 2015) Also, higher Emotional Intelligence (EI) scores over time result in improved performance and decreased resident burnout. (Health Science Journal 2016)
Learn more:
- American Hospital Association: The Impact of Emotional Intelligence and Resiliency on Healthy Care Performance
- Harvard Business Review Emotional Intelligence
Mentorship
Mentorship produces value beyond the creation of good leaders. It contributes to recruitment, retention, and development of the next generation of health care leaders. Effective mentorship has been shown to improve job satisfaction and productivity, facilitate personal growth and career satisfaction, and lessen risk of compassion fatigue and burnout (Leary J., The Unwritten Rules of Mentorship: Facilitators of and Barriers to Effective Mentorship in Pediatric Hospital Medicine Hosp Pediatr 2016). Mentors can lean on their younger colleagues to understand new technology and patient perspective. Finding an effective mentor can support your own path to wellness.
Resources:
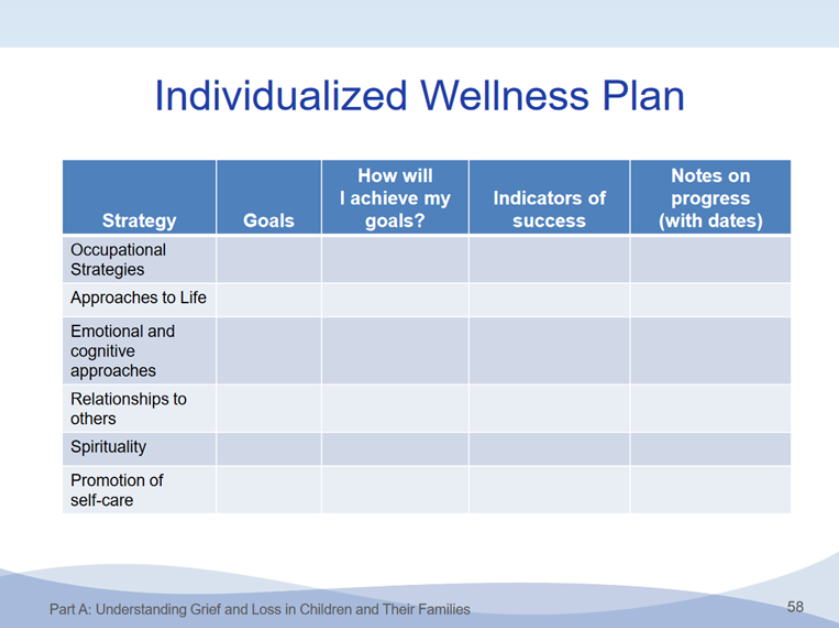
Build your own wellness plan
Developing resilience strategies is key to your ongoing health. Many strategies exist but one size does not fit all. This is a journey that must identify and nurture strategies that meet our individual needs.
Self-care can include multiple concepts. A wellness plan should include strategies for the immediate and long-term situations that will help the individual address the inevitable challenges inherent in health care. Maintaining the joy and passion of practicing pediatrics, despite the inevitable stresses, is a long-term challenge. Developing proactive, healthy life habits can help you maintain your enjoyment of medicine.
- Be aware of personal physical and mental health. Make sure you have a primary care provider, seek medical care when needed, not work when ill, and seek mental health assistance when needed.
- Optimize nutrition.
- Maximize rest and sleep. Keep a regular bedtime routine, minimize distractions, and try to get at least 7 hours of sleep daily.
- Relax, take a vacation, spend time in nature.
- Enjoy hobbies: music, dance, sports, yoga, gardening, photography or crafts, etc.
- Prioritize time for self, partner, family, friends.
For more information, view the “Resilience Curriculum: Resilience in the Face of Grief and Loss,” developed by the AAP Section on Hospice and Palliative Medicine. Part D of the curriculum, “Introduction to Personal Wellness” includes a number of resources for physician wellness.”
Last Updated
01/12/2023
Source
American Academy of Pediatrics